Home / Intravascular Therapies Hub / Implantable Ports
An Overview of Implantable Ports
An overview to medical ports, their placement, and variables to be taken into consideration when selecting your totally implanted vascular access device. (5-10 min read)
Topics Covered:
1. What is a port?
2. When is a port used?
3. Benefits of Ports
4. Port Placements
5. Different types of ports
6. Plastic Vs Hybrid Titanium Ports
7. Selecting a port for a patient
8. Huber Needles for ports
9. Selecting the right port for the right patient
10. Ports and Hubers from Vygon UK
What Is a Port?

Ports are a form of vascular access device that is implanted under the skin of a patient. They can be inserted in various areas including the anterior chest wall, trapezius, and the arm.
Ports are chosen for patients requiring longer term and repeated vascular access and can be left in situ for a period of weeks, months, or years.
Please always refer the advice of the manufacturer for dwell times and placement guidance.
Also known as: Implantable port, Portacath, subcutaneous port, or totally implanted vascular access device (TIVAD)
When is a port used?
Implantable ports have many uses, including:
- Extended Vascular access
- Repeated fluid delivery (including IV Fluids and antibiotics)
- Blood tests and transfusions
- Delivering chemotherapy
- Taking blood samples
You’ll see ports uses in therapies such as: chemotherapy, ongoing treatment of cystic fibrosis, parenteral nutrition, antibiotics, and pain management. Ports can be used in both adult and paediatric patients, with a variety of sizes available to ensure you get the best sizing for your patient.
Benefits of a Port
There are many benefits of using an implanted port for a patient’s therapies that include personal patient benefits, clinical patient benefits and also benefits to the department.
Personal Patient Benefits
Many patients report far more comfort and a feeling of control once having the port placed. Once the port is in situ it is largely un-obstructive, minimally visible, and allows the patient to continue many normal daily activities including bathing and swimming.
Clinical Benefits
Having a port placed is also clinically beneficial for patients requiring longer term IV therapy, or repeated treatments over a period of time. This is due to having a single access point rather than repeat cannulations, which reduces the number of needle sticks and ultimately helps to wards vessel protection.
Studies have shown a lesser rate of infections from port access points than other iv therapies.
Departmental / Hospital benefits
With the patient and clinical benefits this naturally leads to wider departmental and hospital benefits. With the lower rates of infection and other catheter related blood stream infections (CRIBSI’s), ultimately costs less for infection control measures.
Furthermore, once a port has been placed, a patient can often leave hospital to home environments leading to a reduction in hospital stays.
Port Placements
Ports can be placed with the patient under general anaesthetic, or a local anaesthetic can also be used. The placement location of the port is chosen depending on therapy involved and the patient in which it is being placed.
A small incision and ‘pocket’ is made on the chest wall, with the port device placed into the pocket and stitched to the muscle to hold it in place. The catheter is then tunnelled under the skin to one of the main blood vessels and fed through the vein until the tip of the catheter sits just outside of the heart.
Both pocket and incision for the catheter are closed with dissolvable stitches and patients should experience minimal discomfort for 2-3 days after the procedure. After the port has been placed, this is usually left for one week before being accessed and used.
Chest Ports
Traditionally, ports are placed within the chest of a patient, usually in the upper right side. But other placements can also be used depending on the requirements of the patient’s therapy.
Arm Ports
It is also possible to have a port placed in the upper arm area, this is also known as a PICC-port. Suitable for certain patient situations as a chest port may not be suitable in all clinical situations.
As presented by Guanhua et al, there are a few situations where a chest port may not be suitable. For example, chest ports may not be suitable for patients undergoing radiotherapy with chest wall involvement, for instances of breast cancer patients requiring radiotherapy or reconstructive surgeries, as well as patients with radiodermatitis or a compromised respiratory function. Some female patients may also experience ‘bra inconvenience’ and discomfort to the area when a chest port is placed so an arm port would be preferable to enable enhanced patient comfort.
Different types of ports
1. Single lumen
The most common type of port, used for patients receiving only one form of IV therapy at a time.
2. Double lumen
Used for patients receiving two forms of IV therapy at the same time, or need to receive infusions or nutrition during treatment.
3. Power port
These ports are strong enough to work with high pressure injections, such as those required for a CT scan with contrast dye.
4. Differences in materials
There are three types of materials for ports currently in use: titanium, plastic (polyoxymethylene, POM) and mixed (titanium base with a POM shell)
Plastic Vs Hybrid Titanium Ports
Plastic Port Systems
Titanium Ports
Hybrid Ports
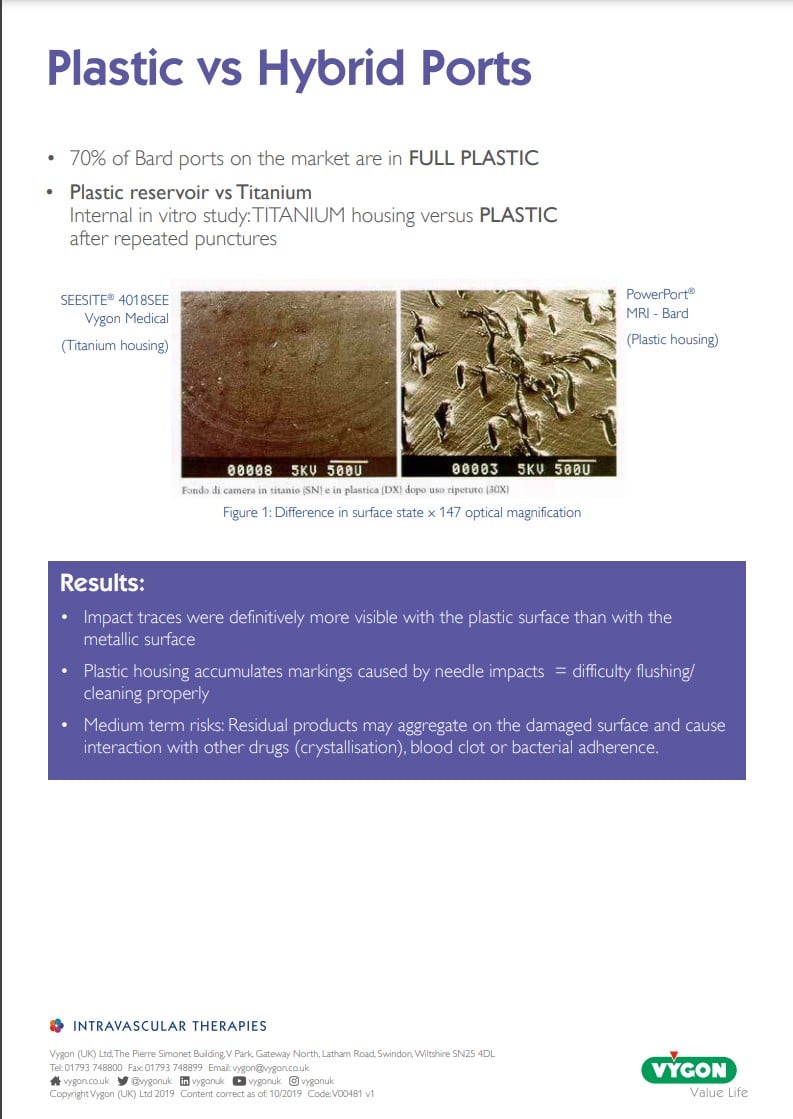
Plastic port systems have the benefit of being lighter in weight and offer the advantage of minimal artefact formation using diagnostic methods such as magnetic resonance imaging.
However, there is some evidence to suggest that plastic ports may also pose a risk for increased incidences of particulate matter build up, due to repeated punctures from Huber needle placement.
In comparison, titanium ports have been the material of choice for many years, as a safe and reliable choice for manufacturer.
But are not suitable for some procedures such as MRI scanning. Resistance against punctures from Huber needle placement is reduced as the material is stronger.
Hybrid ports have the benefits of both material types, with a lighter device that is MRI conditional, yet resists Huber needle puncture and reduces risks of particulate matter build up.
Selecting a port for your patient
When choosing a port for patient placement, considerations should be made for:
1. The age of the patient
Adult and paediatrics will have differing requirements for ports such as sizing and profile of the port. Paediatric ports will need to be smaller in nature.
2. Weight of the patient
With patients who are obese, consideration should be given to the placement and depth of the port depending on the chest fat pad areas in which the port is placed. Whereas with patients with particularly low weight, a picc-port or arm placement may be preferable. (4)
3. Possible therapies/treatment the patient might require
4. Chosen placement on the body of the patient
5. Length of time the port will need to be in situ for.
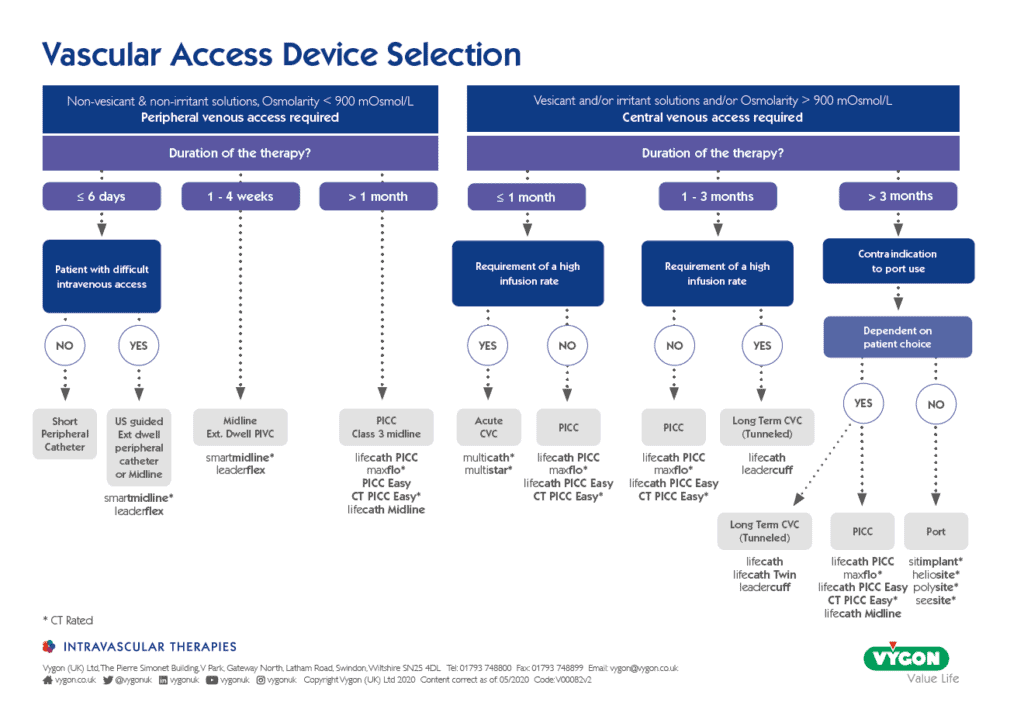
Ports are suitable for IV therapies with 3 months duration or longer.
6. Capabilities of the patient (and their support systems) to care for the port whilst in a home environment.
Huber Needles for Ports

The port is only one part of the system for this vascular access device.
To administer treatment, implanted ports are accessed by introducing a Huber needle. The Huber needle goes through the skin directly above the port.
Selecting the right vascular access device for your patient
Ultimately, it is an important choice of the clinician and clinical care team when selecting the right vascular access device, for the right patient, at the right time. Considerations should be made towards the therapies required, duration of treatment and the preference and experience of patient themselves.
For more information on helping to selecting a vascular access device (VAD), see the Vygon VAD matrix below.
At Vygon UK we have a variety of ports available for both adults and paediatrics and in a variety of sizes from standard, mini and micro. Ensuring you get the right port for the right patient, each and every time.
Seesite™ is an easily administered implantable lightweight, hybrid port for adults and paediatrics requiring injectable medicines.
Available in a variety of sizes.
Polysite™ is an easily administered implantable lightweight, hybrid port for adults and paediatrics requiring injectable medicines.
Available in a variety of sizes.
As vascular access experts, Vygon UK work closely with clinicians and their patients to ensure that our products combine the ideal dwell time – whether that’s short, medium or long-term – with ease of use, effectiveness and value for money.
Our range of ports are specifically designed as totally implantable vascular access devices to deliver secure, long-term intermittent IV therapy. With a focus on patient comfort during a variety of treatments including chemotherapy, parenteral nutrition, antibiotics, pain management, fluids and blood sampling, our ports’ range delivers for both paediatric and adult patients.
Supporting documents
References
- Guanhua Li, Yu Zhang, Hongmin Ma, and Junmeng Zheng ‘Arm port vs chest port: a systematic review and meta-analysis’ Cancer Manag Res.2019; 11: 6099–6112 Accessed at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6613605/
- Weber, D (2022) Combining aesthetics and feasibility in PICC-port placement https://vascufirst.com/ports-and-huber-needles/combining-aesthetics-feasibility-picc-port- placement/
- https://ava2018-ava.ipostersessions.com/?s=C9-1C-FC-EF-64-F1-44-FB-EF-78-21-4B-9E-C8-D2-CC
- https://vascufirst.com/ports-and-huber-needles/combine-aesthetics-feasibility-chest-port-placement/