Home / Intravascular Therapies Hub / Online Resources / Webinars / Peripheral Vascular Access: Webinar questions
Questions and Answers
Amanda Byers, Fluid Nurse Specialist
On Thursday the 27th of May 2021, Vygon hosted a webinar on Peripheral Vascular Access: Understanding the Challenges.
Peripheral intravenous (IV) catheter insertion, the most common invasive hospital procedure performed worldwide, is associated with a variety of complications and an unacceptably high overall failure rate of up to 69% (Marsh N et al VA 2020).
Catheter failure is costly to patients and healthcare providers
Peter Carr presented his research around peripheral cannulas in relation to failure rates, complications, and patient experience.
Amanda Byers presented on her experience at NHS Lanarkshire with the use of midline catheters for extended dwell.
Here are the questions and answers from the webinar:
Q: Which ward / department would you recommend starting in?
A: Our initial planning stage was discussing where to start – looking at areas that have patients who require prolonged IV therapy and therefore, repeated cannulations. We started in our Vascular ward as they had ongoing issues with IV access – patients with poor access and having delays in receiving IV therapy. Our patients can wait up to a week or more for placement of a PICC so if a midline is suitable then it makes sense to use a midline. They very often require IV antibiotics for up to 4 weeks so midlines were perfect for these patients. The other area is Cardiology – patients with conditions that require prolonged IV therapy. They will be our next unit to implement them. You would also potentially use them for patients with difficult access so having a good decision-making tool is paramount in ensuring the patients are having the most appropriate line placed at the right time, be that a PIVC, an EDC, Midline or PICC.
Q: With the difficulties Trusts experience with implementing widespread use of Extended Dwell Catheters, apart from dedicated VA / Radiology teams, which type of clinician do you advise is in the best position to place EDCs within a typical trust?
A: I think, in our Trust, we have many skilled practitioners that can most definitely place EDCs. Our HECT (Hospital Emergency Care Team) team are in the hospital 24hrs a day and are often called on to place cannulas so they will be an invaluable team to be able to place EDC and midlines.
Q: Are the midlines placed within the patients parent ward / bedside or do they go to a designated area?
A: The initial plan was to take patients to a designated area in Theatres for placement. This was more for my supervision and also for ease of having access to the ultrasound machines. Due to Covid, that plan had to change. We have been placing the midlines at the patients bedside (which was the end goal anyway) and it has been working well. The whole point is that they can be placed at the bedside and patients don't need to move to another department. I was fortunate in that I had placed a few lines in ICU first so I was confident enough to move to bedside placement. It's more for the available floor space than anything else but as long as you think about that when you are setting up, it is fine.
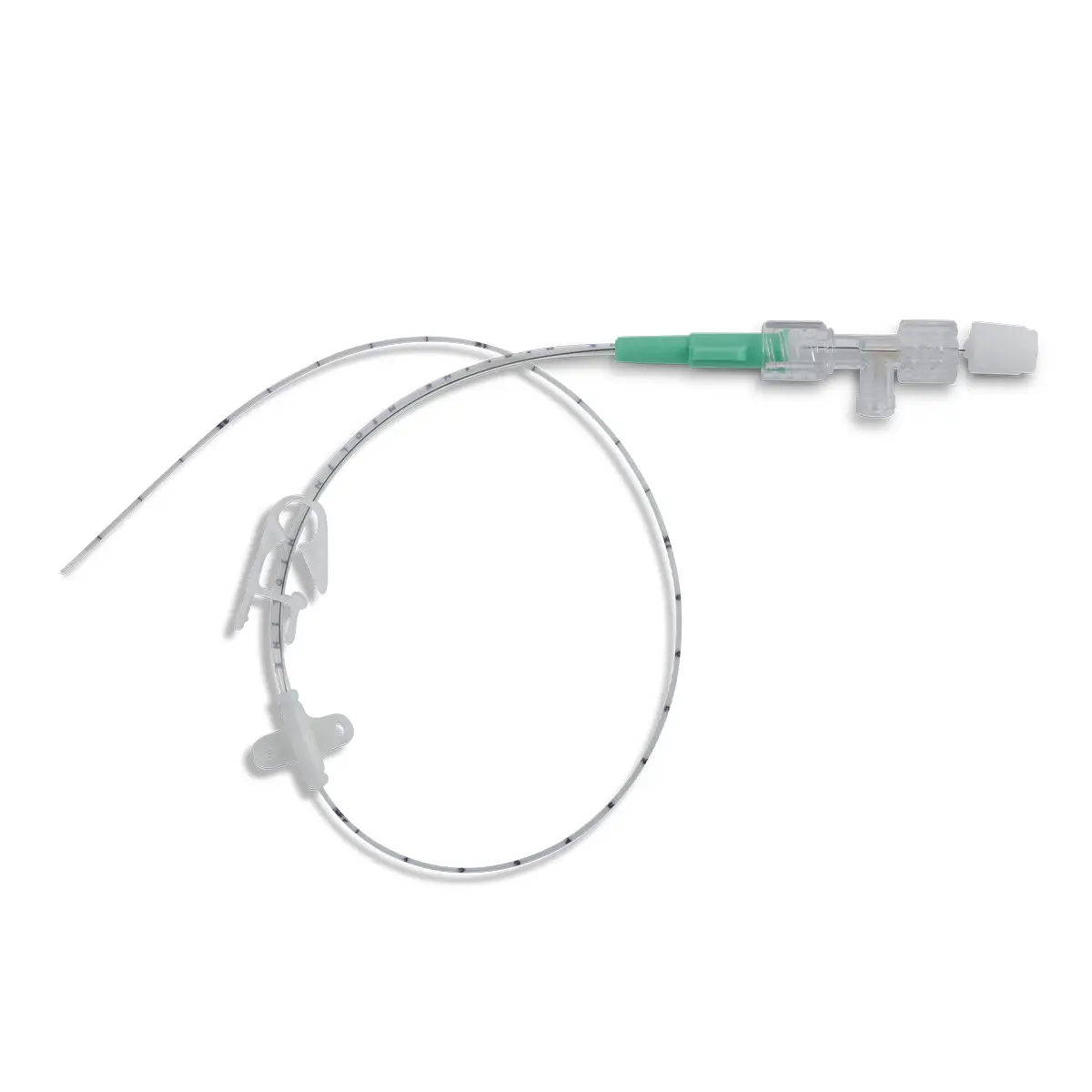
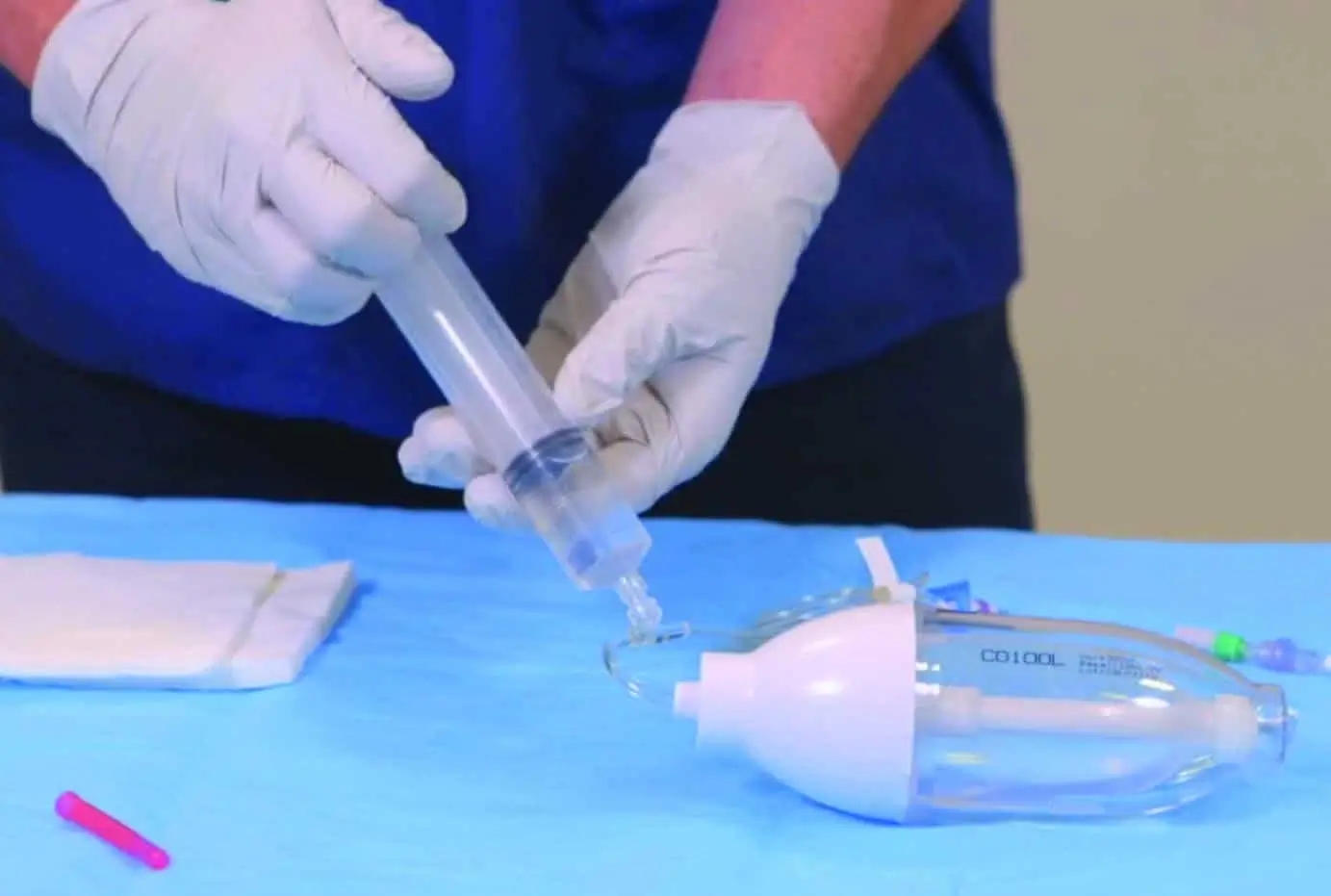
Q: Which midline do you use the most?
A: We have the Smartmidline 6cm 2Fr and 3Fr and 8cm 4Fr. We tend to use the 6cm 3Fr more than the other two. We haven’t had any issues with it so far. We aired more on the side of caution with the length but actually an 8cm would be fine for all the patients we have placed them in so far
Q: How long can the midlines be left in before they need replacing?
A: They can be in place for up to 29 days.
Q: Are the midlines suitable for CT contrast?
A: Our 4Fr Smartmidline is CT rated. We haven’t used any yet as there needs to be more discussions with Radiology for them to be happy to use them so we have just been using the 6cm 3Fr and obviously not recommending them for use in CT. They will be used for CT eventually.
Vygon response: Our Smartmidline catheters are all CT rated up to 325psi with a range of flow rates from 0.5mL/s to 7mL/s depending on catheter gauge size. The 4Fr catheter has a flow rate of 5mL/s.
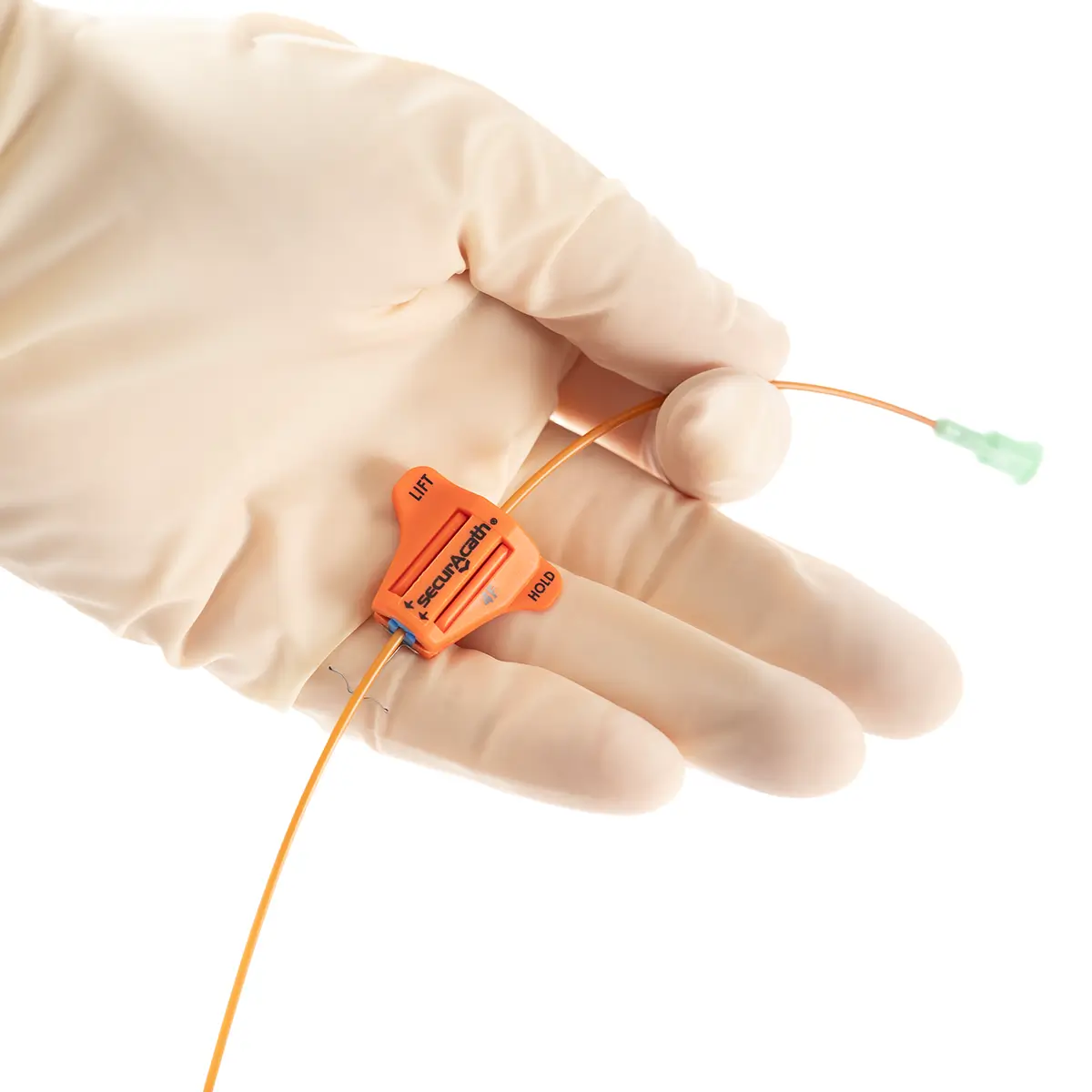
Q: What securement device do you use for the midlines?
A: We use the Grip-Lok securement device directly on the midline and have a transparent dressing over the top.
Q: Do you need an ultrasound for every insertion? We are looking at rolling midlines out for community nurse insertion.
A: If I am using the upper arm then yes you need an ultrasound every time. The extended dwell catheter in the forearm I would put in without an ultrasound as those veins would be palpable.
Q: What strategies would you use if PIVC are being placed as a first option rather than using a device matrix to pick to most appropriate device?
A: I think education is key to roll this out appropriately. Making sure that the areas are aware of the availability of midlines, their use and also to have a robust decision-making tool in place which helps clinicians to choose the correct line for each patient based on their available access, the length of their anticipated IV therapy and also the nature of that therapy. Does it require central access or peripheral?
Q: Is the vascular decision-making tool you use created by NHS Lanarkshire?
A: The vascular decision-making tool was taken from NHS Fife (with their blessing). We simply amended it for our local organisation.
Q: Was there any pushback due to the cost of EDC V Cannula?
A: There was no pushback in regards to cost. When you take into consideration the cost of repeated cannulations, failed cannulations and cannulas that fail during use, the cost of a midline that is looked after and stays in situ for the 28 days offsets the cost variation. Our hospital management were more than happy.
Q: I am a nurse practitioner and place 4Fr midlines which CT will use for contrast also. I feel this is a massive pressure as we get calls to place from all over the hospital. Will your emergency team be placing urgent lines in A&E?
A: The end goal will be for the lines to be placed in ED. When we initially rolled them out in ICU there was a Registrar from ED who was very keen to introduce them. We have a bit of work to do before we are there. We are trying to ensure the wards in the hospital are familiar with the lines and how to care for them properly before we introduce them in places like ED and IR as they will feed directly into the main hospital.
Q: Did IR have any objections to a non-medical led line service?
A: We had a bit of a stumbling block with IR. We had been very open in our discussions early on about our introduction and use of the midlines but when it came to fruition there was a bit of confusion that the midlines would be replacing PICC lines which is obviously not the case. It has sparked further discussions and is resolved now.
Q: Amanda is the role you are in full time? Or is it a number of hours per week?
A: My role is full-time at the moment. It is a seconded post for the National IV fluid programme but we are trying to secure substantive funding at the moment.
Q: Do you think a dedicated IV team is beneficial in Trusts?
A: I think it would be beneficial to have a dedicated team. I think if there was leadership and good processes in place to ensure not only good practice when placing the lines but good care and maintenance, it would surely improve the outcomes for patients.
Q: We are having a number of midline infiltration failures with a 10cm line. How do you manage minimising the length to ensure it ends distal to the axillary vein vs the risk of infiltration / extravasation?
A: We decided to use the 6cm 2Fr and 3Fr and the 8cm 4Fr Midlines. We were erring on the side of caution with the length to make sure we had lines that were suitable for most patients lengthwise. We have only placed the 6cm lines so far and we haven’t had any issues with extravasation. In hindsight the 8cm would have been fine for all the patients we have placed lines in so far.
Q: Patient education and engagement in peripheral device assessment remain important. A prevalence study in Ireland found a significant association between patients unaware of the reason for their device and the device being redundant, predisposing them to avoidable infection. What are the barriers within the workplace that prevent patient education? How can the situation be rectified?
A: I think you make a very good point. I think we need to be very clear on ‘consent’ for these devices. I think we are very good at placing a PIVC just because a patient is in hospital rather than having a good rationale behind it. We are working on this in our surgical receiving ward at the moment. I think we need to ensure we are giving our patients the choice through informed consent, something we are careful to do with the midlines.
Q: How often do the on call Anaesthetists get called to troubleshoot?
A: They have only been called once since we started and that was only because the ward staff robustly followed the guidance on the back of the care plan. It was for removal of a line on a weekend. I am in Monday to Friday so I would take any queries myself during the week.
Q: What is the reasoning behind sending away every tip for the midlines? We only send the tip when we suspect an infection?
A: The decision to send away the tip each time was agreed by the Consultants and also Infection Control. This will only be for a period of time to ensure we are not causing an increase in SABS. We would routinely send away tips of PICC lines and CVCs so they wanted to do the same for the midlines until we are more familiar with them.
Q: Can we not organise a dedicated ” MIDLINE ” expert team in every site, instead of cancelling, for example, a morbidly obese patient or IVDU patient on the day of the procedure?
A: Surely if we have midlines available then your Anaesthetic team, who will be very familiar with ultrasound and Seldinger technique, could place a midline? Would that be the most appropriate line for these patients though?
Q: We really struggle to get clear documentation of failed attempts which I think is really important. Is this important or is it just me?
A: I think it’s important to document failures as well as successes.
Q: Do you have plans to make the care plan electronic or will they stay in paper format?
A: At the moment the care plan will stay in paper format but we are moving to electronic notes so that might change in the future.
Q: In our experience, after 7 days insertion, blood samples are impossible through a midline. Is it the same thing for you?
A: We have written into our SOP that midlines have not to be used for blood sampling. For the stated reason and also the worry of the lines being blocked.
To watch this webinar or others in the bitesize masterclass series, visit the IVT webinar page.