Benefits of Nurse Led Vascular Access

Up to 90% of inpatients require IV access for delivery of fluids, medication and/or blood sampling¹, yet 35–50% of peripheral intravenous catheters (PIVCs) do not meet their intended dwell time, largely due to complications, which can cause delays in treatment and discharge².
Earlier this year we discussed the need for standardisation of care and maintenance of vascular access devices in order to reduce infection rates and complications associated with vascular access devices. Research has shown that when vascular access is required, limited assessment is performed of the most appropriate device to use; PIVCs are often used as the default, despite not being the best device for some patients³.
Up to 50% of PIVCs fail before completion of the intended treatment² and after insertion, there is often little consideration of the survival of the PIVC.
Treatment duration and device dwell times are important factors to consider when selecting an appropriate device for insertion. By choosing a suitable device for the patient’s intravenous needs, repeated cannulation can be avoided, reducing patient discomfort and increasing safety6. Insertion is often delegated to those staff who have the least experience, and who may be unclear of when to escalate issues (and to whom) or when to consider an alternative vascular access device4.
If veins are small, scarred or difficult to find, this can lead to failed cannulation and patients requiring multiple cannulation attempts. The implications for patients of failed cannulation include pain and delayed IV fluids, antibiotics and analgesia resulting in increased length of hospital stay5. A negative cycle of numerous PVCs can also lead to staff frustration and poor patient experience.
Poor quality of peripheral veins often results in escalation to an anaesthetist or interventional radiologist however their time is better spent undertaking more complex clinical work. This along with a shortage of radiologists and a backlog of elective procedures caused by the pandemic, leads to delays in treatment7. Earlier recognition of difficult IV access (DIVA) patients or requiring repeated cannulation allows patients to receive the most appropriate device in a timely manner and reduce complications, treatment delays as well as the associated costs to the healthcare provider6,7,8.
Benefits of Vascular Access teams
Nursing-led vascular access teams specialise in VAD insertion, maintenance, and removal, thereby reducing waiting times, VAD complications and patient outcomes, especially in patients with difficult intravenous access (DIVA)6.
“Nursing-led vascular access teams provide an unimaginably better experience for patients with difficult veins” Barton, 2022
A vascular access nurse can make an early assessment of the patient’s veins and requirements before selecting the most appropriate vascular access device that could stay in for the duration of their therapy.
- In-depth knowledge to optimise device selection
- Reduce healthcare costs through lower resource utilisation and device complications
- Reduce waiting lists & avoid delays.
- Reducing complication rates, including infection, through first attempt success and device care and maintenance
- Educate, audit and perform surveillance to maintain staff adherence to proper care and maintenance
Ports for Oncology
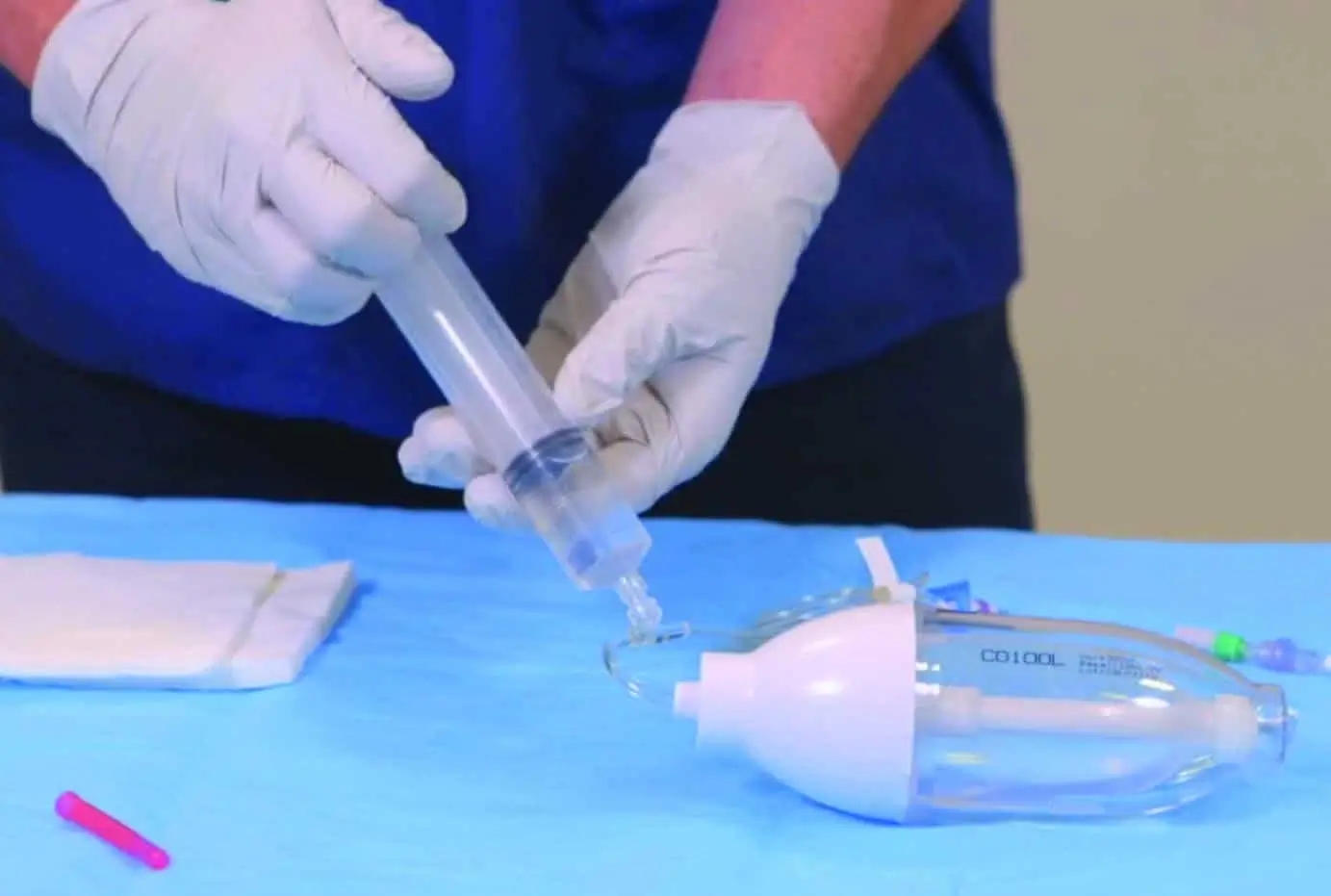
Typical device selection for cancer patients undergoing chemotherapy is a PICC line. Although suitable for the treatment, they can lead to incidences of venous thromboembolism and infections. They can also interfere with a patients daily life, such as bathing, swimming or going on holiday. Totally Implantable Vascular Access Devices (TIVADs) or Ports are often dismissed due to a lack of knowledge or misconceptions by the healthcare professional and patient. Many patients receiving ports can be treated in outpatient settings and can easily be inserted by a nurse using ultrasound or ECG guidance. Nurse-led vascular access teams inserted TIVADs are associated with increased patient satisfaction, lower risk of complications and lower maintenance, making them a more suitable option and more cost efficient based on the duration of therapy9,10,11.
‘For most patients receiving [systemic anticancer therapy], PORTs are more effective and safer than both Hickman and PICCs. Our findings suggest that most patients receiving [systemic anticancer therapy] for solid tumours should receive a PORT within the UK National Health Service.” CAVA Trial
Training from Vygon
Our clinical nursing team and product specialists are able to provide a wide range of training and support to suit your requirements. We run on-site training and education as well as hosting yearly TIVAD insertion courses for those looking to implement nurse-led vascular access teams. To ensure you get the best out of your service, Vygon is on hand to support you every step of the way. We not only offer a full range of vascular access devices but are available to advise on clinical training and support, as well as patient guidance.
Contact us today to discuss how we can support you.
Vascular Access
Always ensure the right line, for the right patient, at the right time – every time. Vygon UK provide an outstanding range short, medium and long term vascular access devices.
From PICCs, midlines, ports and hubers to Elastomeric Devices and ECG tip location systems to help you to plan and achieve the correct intravascular therapy for improved clinical outcomes.