How can Vygon’s products align your practice with the new 2025 ESAIC Guidelines on Intra-operative Haemodynamic Monitoring and Management?

Introduction
Intra-operative haemodynamic management is a cornerstone of safe and effective surgical care. The 2025 guidance from the European Society of Anaesthesiology and Intensive Care (ESAIC) provides updated, evidence-informed recommendations for clinicians managing adult patients undergoing noncardiac surgery. This article distils the key points from the new guidelines and highlights how Vygon's innovative solutions align with and support these recommendations.
Core Principles of the Guidelines
The ESAIC panel, comprising 25 international experts, focused on seven key areas:
- Arterial Pressure
- Heart Rate
- Stroke Volume and Cardiac Output
- Cardiac Preload and Fluid Responsiveness
- Echocardiography
- Microcirculation
- Depth of Anaesthesia and Cerebral Oximetry
1. Arterial Pressure
- Primary Target: Maintain mean arterial pressure (MAP) above 60 mmHg.
- Measurement: Continuous invasive monitoring in high-risk patients is preferred; otherwise, oscillometric methods with proper technique are used.
- Individualisation: Consider patient-specific baseline pressures, especially in those with chronic hypertension.
- New Technologies: Continuous non-invasive monitoring (e.g., finger-cuff systems) is promising but not yet standard.
Key Takeaway: MAP is the most reliable indicator for guiding intra-operative blood pressure management.
Arterial Pressure Management
ESAIC Quote:
"Compared with intermittent oscillometric monitoring, continuous arterial pressure monitoring with an arterial catheter can help clinicians detect and reduce hypotension1."
Vygon Solution:
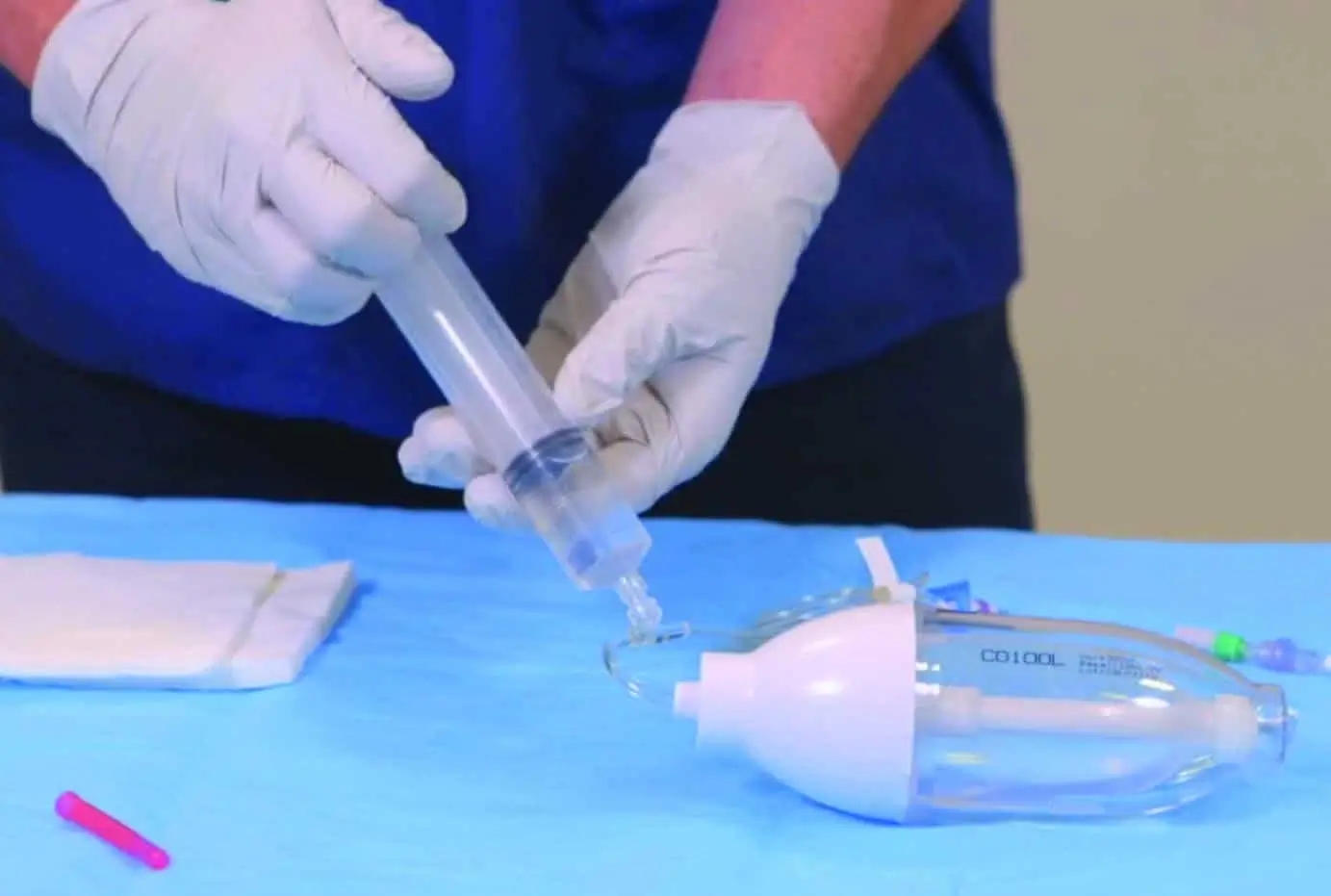
Leadercath – Vygon's arterial catheter system enables accurate and continuous arterial pressure monitoring, supporting early detection and management of hypotension during surgery.
Materials and Methods
ESAIC Quote:
"To minimise the risk of complications, we recommend primarily inserting arterial catheters into the radial artery and using small-diameter arterial catheters (20 G) 1."
Vygon Solution:
Leadercath – Designed for radial artery cannulation, this catheter supports guideline-compliant practice with minimal invasiveness and high safety.
Ultrasound-Guided Insertion
ESAIC Quote:
"Clinicians may consider inserting arterial catheters in the radial artery using ultrasound guidance to increase the first-attempt success rate 1."
Vygon Solution:
Vysion Andy – A handheld ultrasound-guided probe to assist in arterial line placement, enhancing first-pass success and reducing complications
Dynamic Response and Signal Accuracy
ESAIC Quote:
"Catheter-tubing-transducer systems must be checked for an adequate dynamic response to avoid measurement artefacts caused by underdamping 1."
Vygon Solution:
Mostcare Up – Automatically detects and corrects underdamping, ensuring accurate arterial waveform readings and reliable haemodynamic data.
Identifying and Treating Hypotension
ESAIC Quote:
"We recommend identifying the underlying causes of intra-operative hypotension and addressing them appropriately 1."
Vygon Solution:
Mostcare Up – Provides real-time, continuous assessment of haemodynamic response to interventions, helping clinicians tailor therapy to the underlying cause.
2. Heart Rate Monitoring
- No Universal Thresholds: Bradycardia (<60 bpm) and tachycardia (>100 bpm) should be treated based on clinical context.
- Treatment Strategy: Intervene if abnormal heart rates cause hypotension or compromise perfusion.
Key Takeaway: Focus on the haemodynamic impact of heart rate changes rather than fixed numerical thresholds.
3. Stroke Volume and Cardiac Output
- Monitoring: Recommended in high-risk patients or high-risk surgeries.
- Avoid Routine Maximisation: Do not aim to maximise cardiac output universally; tailor targets to individual needs.
- Goal-Directed Therapy: Should be personalised and based on clinical and metabolic signs of perfusion.
ESAIC Quote:
"We suggest monitoring stroke volume or cardiac output in patients with high baseline risk for complications or in patients having high-risk surgery1… "
Key Takeaway: Cardiac output monitoring is useful but must be linked to meaningful therapeutic decisions.
Vygon Solution:
Mostcare Up – Powered by PRAM technology, offers real-time, beat-to-beat hemodynamic data without external calibration. Enabling clinicians to detect subtle changes in stroke volume and cardiac output, make informed decisions based on dynamic parameters, and personalise treatment strategies to optimise perfusion and outcomes.
Avoiding Overuse of Invasive Technologies
ESAIC Quote:
"We suggest considering these invasive monitoring methods to measure cardiac output in selected patients with severe cardiopulmonary comorbidities (e.g. severe left-sided or right-sided heart failure, pulmonary hypertension) or in patients having noncardiac surgery with particularly high risk (e.g. liver transplant surgery) 1."
Vygon Solution:
Mostcare Up – Provides (minimally invasive) advanced haemodynamic monitoring without the need for central venous or thermodilution-based systems, aligning with the guideline's preference for less invasive, high-utility tools.
4. Fluid Management and Responsiveness
- Assessment Tools: Use dynamic indicators like pulse pressure variation (PPV) and stroke volume variation (SVV) with caution.
- Fluid Challenges: Should be guided by stroke volume or cardiac output changes.
- Avoid Overuse: Do not administer fluids solely based on fluid responsiveness; look for signs of hypovolaemia or hypoperfusion.
Key Takeaway: Fluid therapy should be judicious, evidence-based, and responsive to real-time physiological needs.
Vygon Solution:
Mostcare Up – Fluid Management offers real-time, beat-to-beat monitoring enables accurate tracking of stroke volume and cardiac output during fluid challenges with immediate feedback on the effectiveness of fluid administration, helping to avoid fluid overload by ensuring interventions are based on meaningful physiological responses.
5. Echocardiography
Echocardiography provides real-time imaging of the heart, enabling clinicians to assess cardiac anatomy and function. It is particularly valuable for diagnosing the causes of haemodynamic instability during or after surgery and can help identify conditions such as:
- Hypovolaemia
- Left or right ventricular dysfunction
- Cardiac tamponade
- Valvular dysfunction
- Pulmonary embolism
Key Takeaway: Recommend performing focused transthoracic or transoesophageal echocardiography as a diagnostic tool for patients developing haemodynamic instability during or after surgery.
6. Microcirculation
- Current Limitations: Sublingual microcirculation monitoring is not recommended for routine use due to technical and interpretive challenges.
- Surrogate Markers: Use lactate levels and central venous oxygen saturation to infer tissue perfusion.
Key Takeaway: Focus on global indicators of perfusion until more practical microcirculatory tools are validated.
7. Depth of Anaesthesia and Cerebral Oximetry
- Processed EEG: Helps titrate anaesthetic depth and reduce haemodynamic side effects.
- Cerebral Oximetry: Not recommended for routine use but may be helpful in high-risk patients.
Key Takeaway: Neuromonitoring supports haemodynamic stability and may reduce postoperative complications like delirium.
Summary: Vygon's Alignment with ESAIC 2025
| ESAIC Recommendation | Vygon Product |
| Continuous arterial pressure monitoring | Leadercath |
| Radial artery 20 G catheter | Leadercath |
| Ultrasound-guided insertion | VysionAndy |
| Avoid underdamping | Mostcare Up |
| Identify hypotension causes | Mostcare Up |
| Monitor SV/CO in high-risk patients | Mostcare Up |
| Avoid overuse of invasive technologies | Mostcare Up |
| Stroke Volume and Cardiac Output | Mostcare Up |
| Fluid Management and Responsiveness | Mostcare Up |
Conclusion
The 2025 ESAIC guidelines emphasise a personalised, evidence-informed approach to intra-operative haemodynamic management. Vygon's suite of monitoring and arterial solutions is well-aligned with these recommendations, offering clinicians the tools they need to deliver safer, more effective care.
For any further information on these guidelines, you can visit the European Society of Anaesthesiology and Intensive Care website here: https://esaic.org/
References
[1] Saugel, B., Buhre, W., Chew, M. S., Cholley, B., Coburn, M., Cohen, B., ... & Zarbock, A. (2025). Intra-operative haemodynamic monitoring and management of adults having noncardiac surgery: A statement from the European Society of Anaesthesiology and Intensive Care. European Journal of Anaesthesiology, 42(7), 543–556. https://doi.org/10.1097/EJA.0000000000002174