Mostcare Up Haemodynamic Monitor: Interview with a user
Find out how out Dr Maria Occio Ferrao, introduced MostcareUp haemodynamic monitor into her department.
Dr Maria Occio Ferrao (Rocio), Consultant Anaesthetist at Norfolk and Norwich University Hospital Trust, introduced MostcareUp haemodynamic monitor into her department in May 2019.
In 2022, we hosted a round table event, in which Rocio presented on a series of case studies surrounding the treatment of gynaecological cases and how the use of a haemodynamic monitor resulted in reduced stay and improved patient outcomes. To view the case study, click here.
Norfolk and Norwich NHS Trust are one of the few Trusts that conduct Ovarian HIPEC (hyperthermic intraperitoneal chemotherapy) in the UK which gives patients aggressive cancer treatment with the aim of curing them of peritoneal cancer deposits. During this procedure, the surgeon will remove all visible tumours within the peritoneal cavity. The peritoneal cavity will then be washed out with warmed chemotherapy. This is to eliminate any disease that is too small to be seen and that could be left behind during conventional surgery. The length of the surgery is between 6 and 12 hours.
While at our HQ, we were able to interview her regarding her experiences introducing MostcareUP into her practice.
Q: What would you say is the reason you chose Mostcare over the other haemodynamic monitors on the market?
So, because my intensive care colleagues were testing and trying Mostcare in the Intensive Care Unit. So we, in the Anaesthetic Department, we were trying a different monitor. We did have an agreement that whatever monitoring we went with would be the same in both departments. So, my Intensive Care colleagues suggest that I try the Mostcare and then they were going to try the other monitor.
Q: And what would you say are the key features with Mostcare that you really like? And how do those impact a lot of the cases that you use it for?
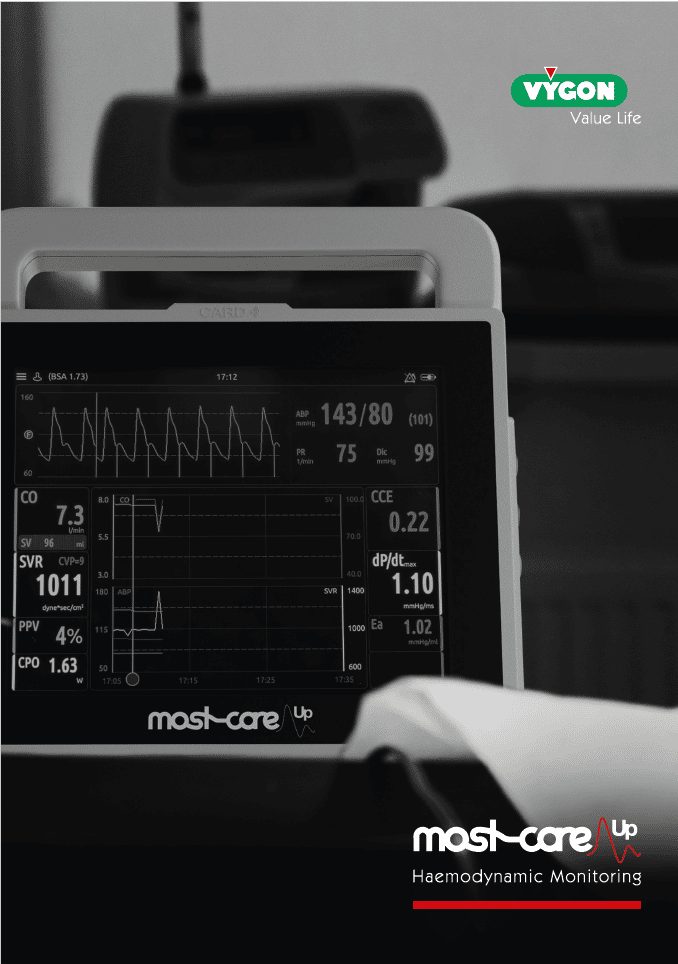
I like that you can assess every part of the cardiac output variables and it is assessed by the monitor. So, it’s not just looking at the three variables that other monitors assess, they only look at the Cardiac Output, Stroke Volume Variation and Systemic Vascular Resistance, I like that you got other variables that you can assess, the afterload, the contractility, the preload and there are more variables that ICU use but I don’t.
So overall, Mostcare gives you a better picture how to treat your patients and you can target therapy to the patient.
Q: Who are the key users of Mostcare within your hospital apart from yourself?
So, the group that do the Gynaecology cases, so the seven Consultants who do these cases another one on the basis they use it. We started using them more in emergency cases with laparotomy, and sicker ones because they get more comfortable. And now Intensive Care after seeing the improvement on the care and the improvement in the outcome of these patients, they’re now trialling it as well and they go back to it, and I think they’re quite keen to introduce it into the normal practice in Intensive Care.
Q: How did you go about bringing all of those different people on board?
It’s an element of training. So, they need to feel confident using the machines, but they also found once they started using it on the cases, then they realized that the practice had changed, it was easier for them to manage these difficult, challenging cases. And actually, the patients do better. And because it’s a small group to start using it, they noticed a difference and they started to see that they were having better outcomes on the patients that they were using the Mostcare to manage to their care.
So that’s why. Just the results.
Q: How would you say the introduction of Mostcare has changed your practice or the service that you offer?
Actually, it’s changed a lot. I know the first thing is, reduced stress. Dealing with difficult cases where you don’t know where you are from a cardiovascular point of view or the cardiac point of view, and you can do a high-risk procedure, that the chance to have this tool that will help you to assess, obviously reduce your stress and help you, it is a really good tool to manage these difficult cases. And, you know, on the on the regular cases, that we do like Ovarian Cancer, the fact that they’re doing really good afterwards and it’s making a difference. And that is really, really grateful.
Q: Is there anything that you think that Vygon could have done better as a provider, a supplier and as a partner?
No, actually, I think I firmly choose to support it. They provide the training course that we went on and we were able to see it in action, the fact that you can put it the monitor into simulations and then you can safely mock different cases in a sim. Having different people who are experts in fluid management and can help you understand, because it’s really difficult about talking about fluid management and cardiovascular monitoring, so having the support it was amazing. Absolutely amazing.
Also, we did have a struggle to get the money to buy the monitor and having all the data to try to support that and being patient with us allowing us to keep the machines when we went through the process to show the managers that it was making a difference, that was invaluable.
Q: What would you say has been your biggest challenge to get you from where you started with haemodynamic monitoring to where you are today?
Well, the biggest challenge was convincing my other colleagues, So the high levels in the departments, the SD and the divisional leads and the intensivists. So, the intensive care colleagues did not believe in noninvasive cardiac output monitors. They had a quite clear view. So obviously my strategy was that I have to show them that it actually does make a difference. I needed to analyze data and put something in front of them.
I made sure to keep a record of the data and then once I showed it to them, then they couldn’t say it was just the number generator. And now they’re keen to introduce it in the ITU practice, that’s told you everything about how the culture has changed and so
I think you if you analyze your data and you see that the things that you’re doing when you change something is positive, it’s not because I like, it it’s because its making a difference.
Q: What would you say is one of the most important factors that you consider when you’re looking at introducing haemodynamic monitoring or cardiac output monitoring?
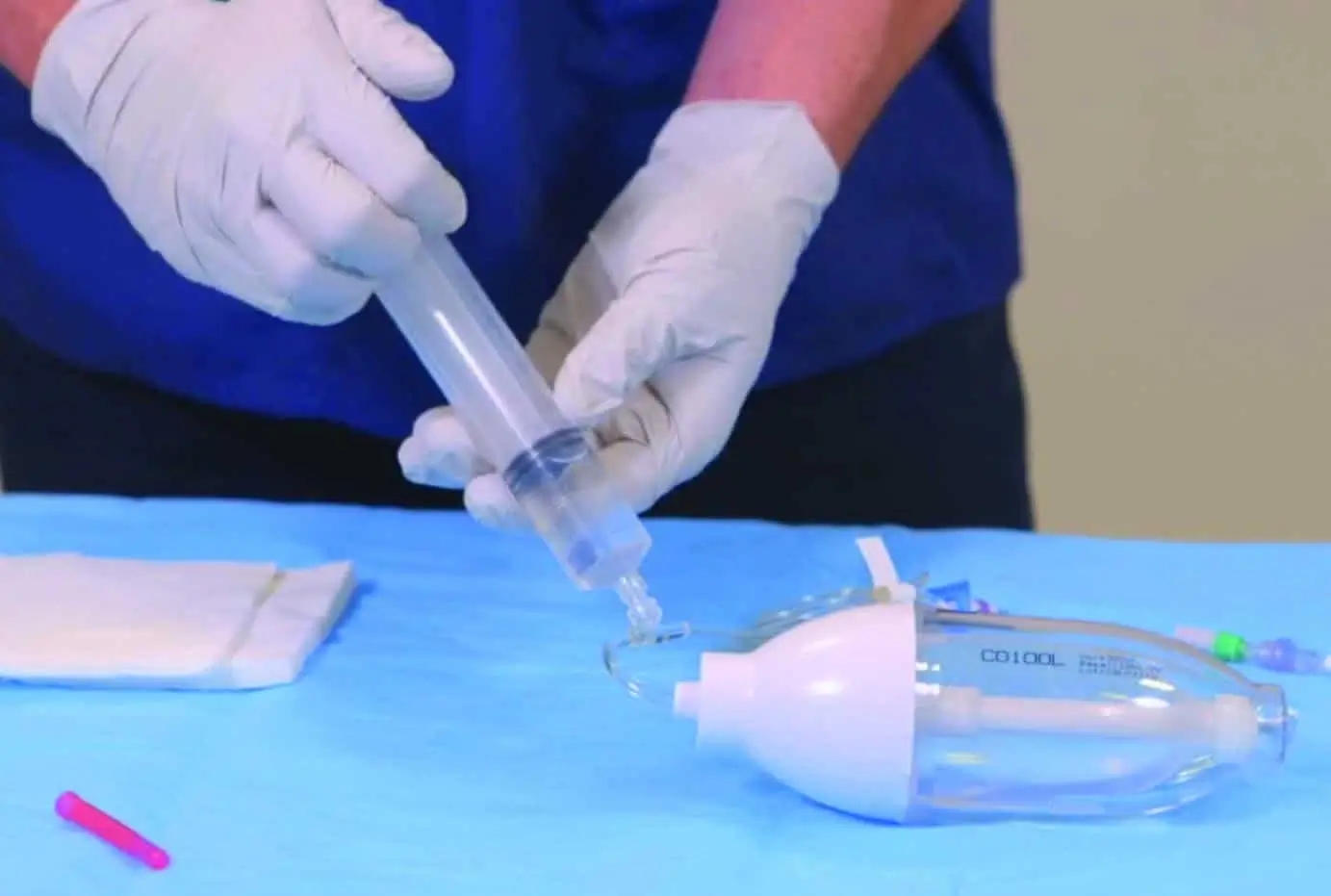
You know, I’ve done that in hindsight. The insight is it that it has to be easy to understand by people. Yeah. That is the key. If you’ve got difficulty, in terms of setting it up, difficulty to interpret what the monitor is telling you or how to do different functions in the monitor to guide your practice, then is going to take you much longer to introduce the product.
But if it’s simple and you can do it quickly. And actually, you’re talking about basics, you’re talking about physiology parameters, and they are, that everybody understands and then you apply it to the monitor because you say it’s so easy to use then that is a winning point in that case.
Mostcare Up is a haemodynamic monitor for use in both adults and children and can be used in a wide range of clinical environments from the ICU and high risk surgery to A&E.
Follow this link to find out more or use the form below to make an enquiry about introducing Mostcare Up haemodynamic monitor to your department or trust.
MostcareUp Downloads & Resources
Contact Us
If you would like to speak to a Vygon representative regarding Mostcare Up or how our team can support your Trust, please complete the form below.