6 Core Principles of Vascular Access Care & Maintenance

Vascular access devices can be found across many hospital departments and patient pathways as a crucial element of providing intravascular therapies. This means that a wide range of clinicians can encounter even a single device, which can risk deviation in maintenance procedures.
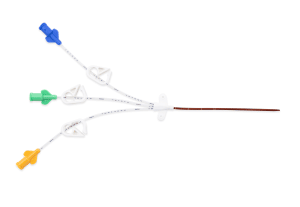
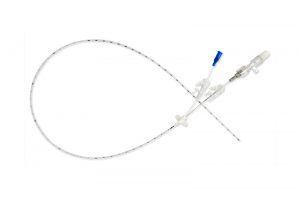
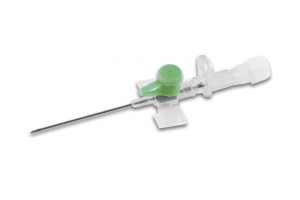
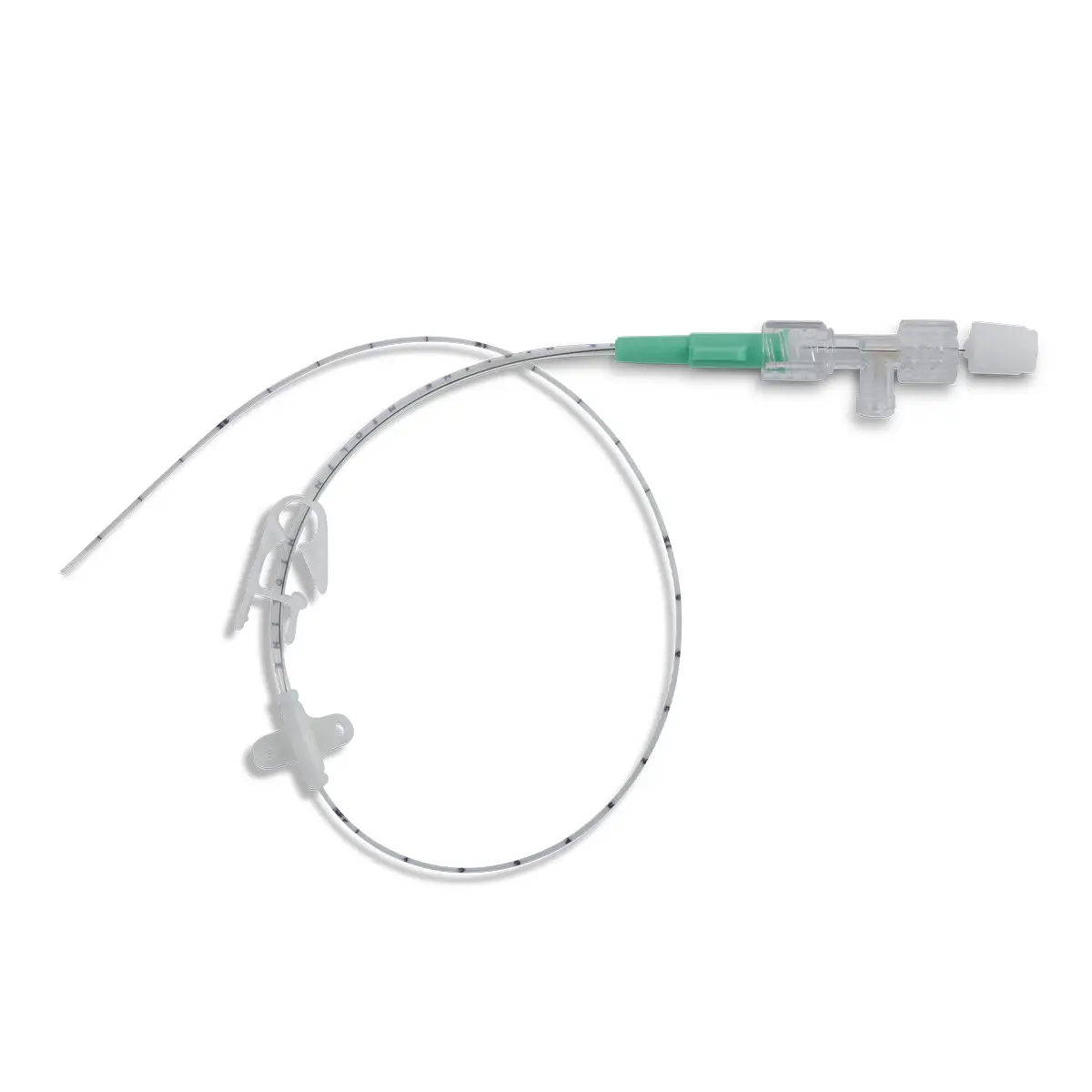
Vascular Access Devices: This term covers everything from basic catheters, and peripherally inserted central catheters (PICCs) to, midlines and central venous catheters (CVCs). These devices are a vital part of intravascular therapy and can remain in-situ throughout a patient’s hospital stay and even during outpatient treatment.
Deviation in care and maintenance practice could lead to opportunities for increased infection risks and complications.
Possible complications of vascular access devices include:
- Occlusion (including mechanical, chemical, thrombotic and persistent withdrawal)
- Phlebitis
- Drug infiltration and extravasation
- Infectious complications
- Dislodgement
Here at Vygon UK we promote the 6 Core Principles of Vascular Access Care & Maintenance. With the view to help better standardisation of practice for clinicians who come into contact with a vascular access device.
6 Core Principles of Vascular Access Care & Maintenance
1) Choosing the right line for the patient from the outset
2) Hand-washing best practice
3) ANTT® : Aseptic non-touch technique
4) Needle-free devices and active disinfection
5) Dressing and regular monitoring of vascular access sites
6) Adequate catheter clearance
Choosing the right line, for the right patient at the right time
Upon patient admission, selecting the right line for the patient can help with their journey and ultimately how the device is cared for and maintained throughout placement.
Considerations should be made for the patient-specific clinical conditions, and the following factors should be taken into account before choosing and placing a line. For example:
- Is it a vesicant or irritant solution?
- What is the osmolarity of the solution?
- How long is the therapy anticipated to last?
By selecting the right vascular access device from the outset, this helps to prevent repeat cannulations which can increase the risk of infection. This practice also proactively supports timely clinical intervention, reduces vessel damage, and preserves vessel integrity.
For more information on choosing the right vascular access device, see the handy Vygon Vascular Access Device Selection matrix.
Handwashing best practice & ANTT®

When placing, or interacting with the device, a clinician should always refer to handwashing best practice and refer to the aseptic non-touch technique (ANTT) ®.
If a patient is being treated in an outpatient setting, or is using a self-administration vascular access device, ensure they are advised of, and adequately trained on correct handwashing technique to prevent complications.
Needle-free devices and active disinfection
Needle-free devices are a vital medical component that attaches to the end of vascular access devices. Clinicians should be aware of the differing devices available on the market, how their design and internal functionality can impact their associated risks of infection and the importance of active disinfection – or ‘scrubbing the hub’ as its more often known.
Clinicians must also note that needle-free connectors should be changed as per the manufacturer’s recommendations[1].
Discover the leading range of Needle Free Devices from Vygon.
Including our market-leading Bionector – the neutral displacement needle free connector.
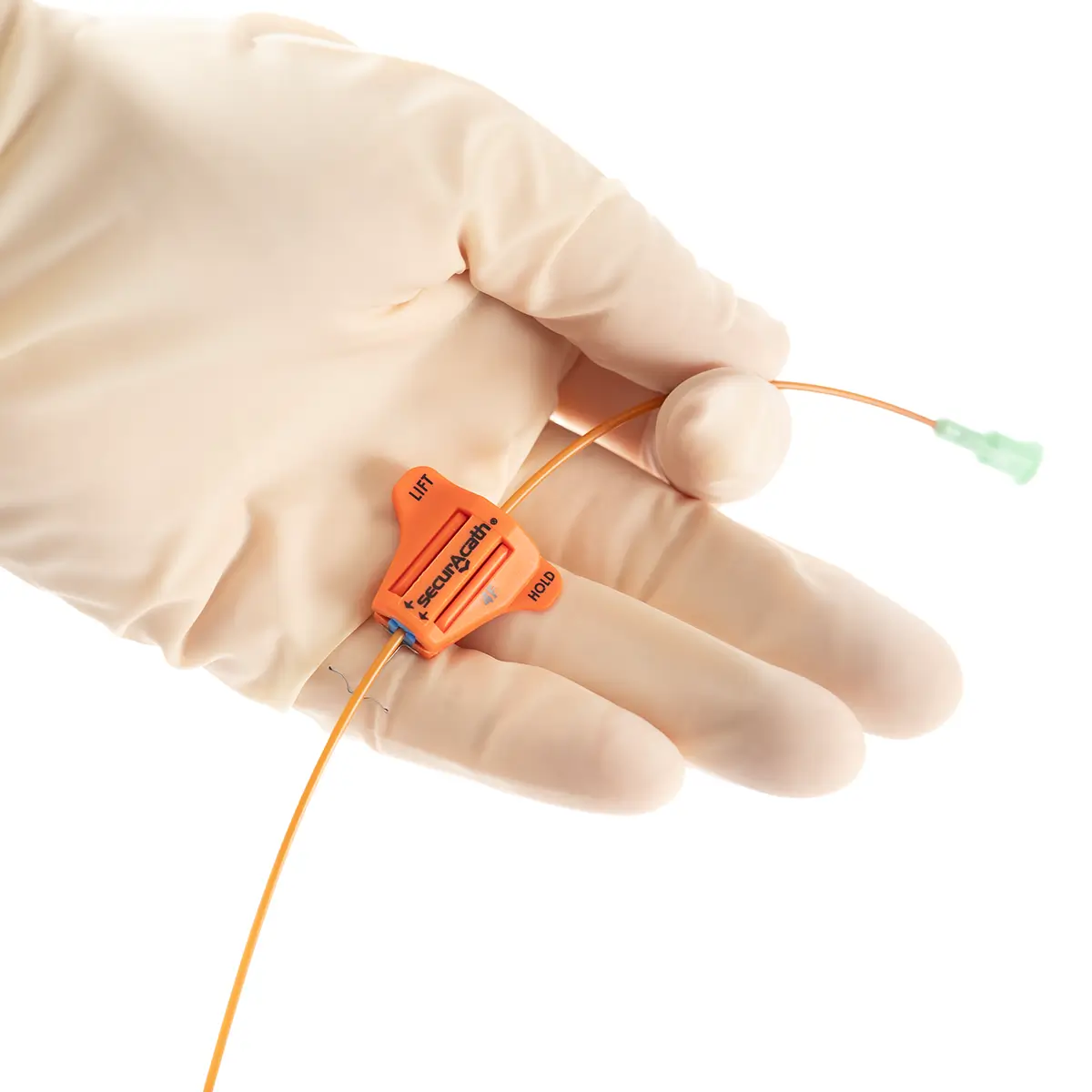
Dressing and regular monitoring of vascular access sites, patient education and advocacy
There are multiple functions of dressings, including;
- Providing security for the catheter to prevent dislodgement.
- Creating a barrier impermeable to water and bacteria.
- Protecting the catheter site from extrinsic contamination and discourage bacterial production at the insertion site.
Dressings should be transparent to allow visual inspection of the site, they should be self-adhesive and provide stability, thus reducing the risk of vein intima trauma, phlebitis and contamination.
A sterile transparent film dressing must be applied and maintained on vascular access devices.
All dressings must be changed at established intervals in accordance with organisational policies/procedures and manufacturer’s guidelines, and immediately if the integrity of the dressing is compromised.
Furthermore, regular monitoring of vascular access device sites is crucial, as is the ability to spot the warning signs of such issues. As with any infection prevention, early intervention is key.
A case can also be argued for increased patient education and self-advocacy relating to vascular access devices. This can be done by raising patient awareness on the core signs and issues they may see around site, when a vascular access device is on their person, and alerting medical professionals for earlier intervention.
Signs can include:

Visual indications
IE Redness around the area, swelling, etc,

Physical indications
IE Warmth surrounding the area, or increased pain reported by the patient

Administrative Indications
IE increased pressure required when flushing.
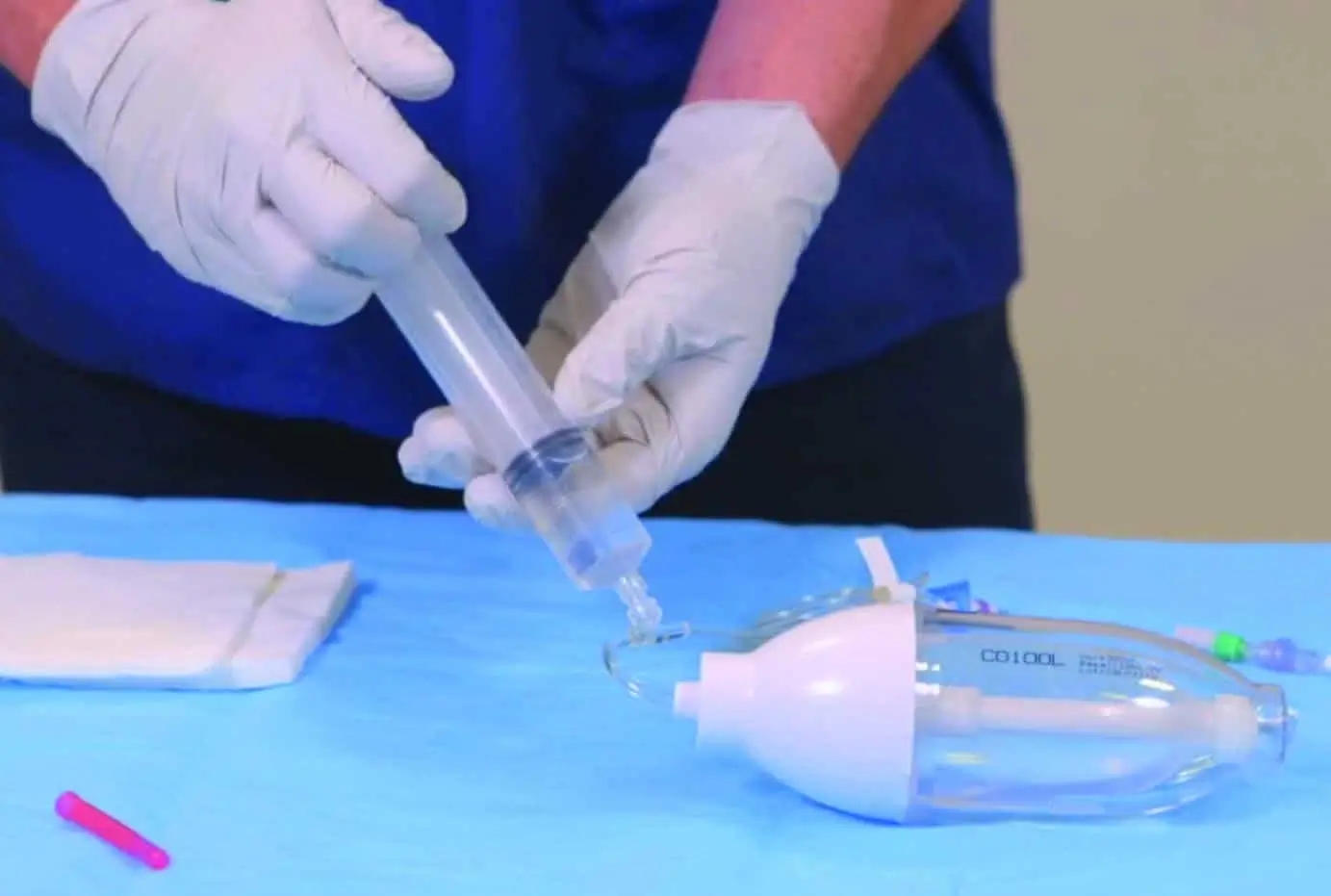
Adequate catheter clearance
The flushing of catheters is one of the most important preventative measures used to prevent occlusion which should be done at regular intervals to promote and maintain patency and prevent the mixing of incompatible medications and/or solutions.
Protocols for flushing should be established within each organisation, but here is some useful guidance on flushing:
- A vascular access device should be clamped after completion of the final flush to decrease the risk of intraluminal occlusion
- Catheters should be flushed with 0.9% normal saline
- A turbulent flush should be used by using a ‘push/pause’, stop/start technique and positive pressure clamping sequence. This helps to remove debris from the internal catheter wall.
- Positive flushing prevents reflux of blood into the catheter tip, reducing the risk of catheter occlusion. This is accomplished by maintaining pressure on the plunger of the syringe while clamping or disconnecting the syringe from the needle-free device – this is particularly important when using a negative pressure needle-free device.
- Syringes used for flushing of central venous access devices should be no smaller than 10ml. Smaller syringe sizes will generate excessive pressures and could lead to catheter fracture.
- Do not forcibly flush any vascular access device. If resistance is met and/or no blood return noted, take further steps to locate the cause of the obstruction (check closed clamps or kinked sets, removing dressing).
Vascular access devices and training from Vygon UK
Although we cannot fully eliminate the risk of complications and infection, by standardising these care and maintenance practices we can all work to reduce the risk and thus improve outcomes for patients.
Here at Vygon we specialise in providing a wide range of medical devices for vascular access. Along with our products we also provide staff training and education as a core part of our offering.
We understand the need for regular training for all healthcare professionals that can be delivered in a way that best suits the departmental and individual needs. Whether this be on-site training within the department or Trust, workshops, or e-learning so an individual can study at their own pace. We even offer a CPD-accredited competency.
Through the delivery of our vascular access devices, we place an importance on partnership with the Trust to help them with standardisation of training and practice throughout departments, governance, and quality improvement projects.
We offer mentorship within the clinical areas and support via our intravascular hub and from our team of clinical educators who have many years of experience within the speciality.
Vygon UK Vascular Access Devices
For more information about any of our vascular access device ranges, see the links below, or get in touch with a member of our team for more information.