Home / Intravascular Therapies Hub / Acute to Community
Acute to Community: Out of Hospital Care
A significant proportion of patients in hospital beds have excess lengths of stay and could be looked after in an alternative setting.
Over the last 30 years, the number of hospital beds has more than halved. At the same time, hospital admissions have been rising. It is estimated that up to 50% of beds are occupied by people who could be cared for in community settings.1

Counting the Cost of the Challenges
The last eight years have seen steady growth in all areas of hospital activity:
- Emergency admissions have risen by 14% since 2008/9
- For planned care, elective admissions are up 22%
There are 15 million people living with long-term conditions and over 2 million with multiple long-term conditions. Together they account for 77% of inpatient bed days. These trends are likely to be magnified in the future by demographic and epidemiological pressures.1
There is no doubt, pressure on NHS resources is considerable and continuing to escalate. An excess bed in the NHS costs between £2,089 and £2,532 a week for non-elective and elective inpatients, respectively.2
The NHS Long Term Plan outlines a commitment to Out of Hospital (OOH) care by increasing investment of £4.5B in primary medical and community health services across 5 years to 2023/24. The aim is to create a fully integrated community-based healthcare system.3

Benefits in Delivering OOH Care

Evidence suggests that OOH healthcare, when delivered well, can provide considerable benefits for both patients and healthcare providers.
Potential benefits to patients and healthcare providers include:4,5,
- Improved patient experience
- Better management of chronic conditions
- Improved resilience and self-care
- More co-ordinated care
- Fewer admissions
- Lower waiting times.
For patients, quality of life, patient satisfaction, and treatment compliance have been found to be overwhelmingly higher when patients receive their care in the community rather than an acute hospital setting.6,7,8
OOH services offer a much more personalised approach to care, allowing relationships to form which engender confidence in patients to manage their condition and undertake the treatment offered.
By spending less time in the hospital, the impact on day to day life is dramatically reduced. This has a consequential impact on the patient’s ability to undertake and remain in employment; it can support children and families to access education more consistently and the person maintains their community links which may support others.
For Healthcare Providers, there are potential cost efficiencies in delivering care in alternate settings. Trusts can also focus integrated services on those patient groups most likely to derive the most benefit.
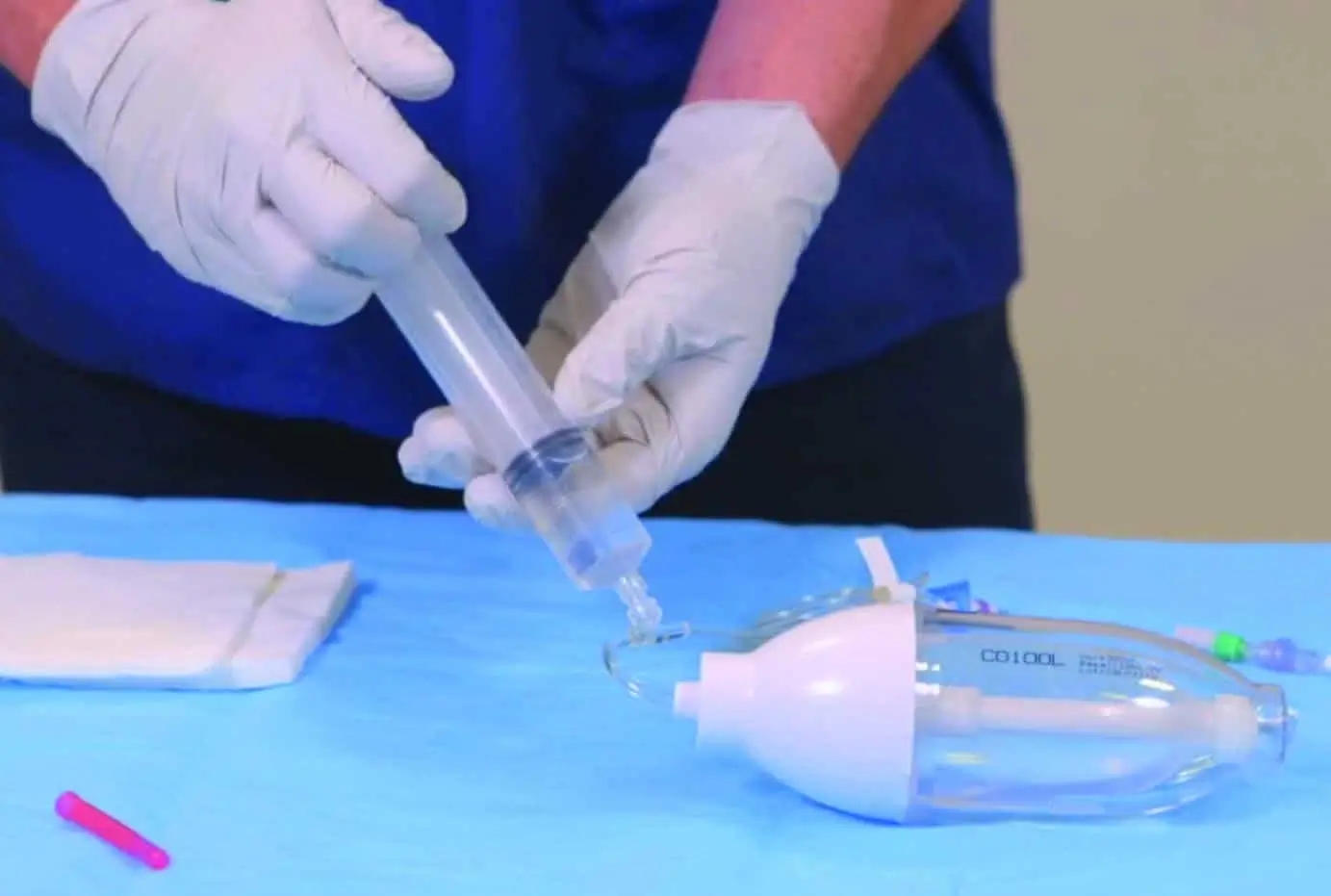
An example of a successful pilot programme is the British Heart Foundation funded evaluation of the treatment of heart failure patients in the community with intravenous diuretics.
This was a two-year project with 10 NHS organisations across the UK to determine whether funding a home or community based intravenous (IV) diuretic service is safe, clinically effective, cost-effective, and well received by patients and carers.
“© British Heart Foundation, [2020]. Reproduced with kind permission of the British Heart Foundation.
The Increasing Demand for Out of Hospital Care
Part 1
A significant proportion of patients in hospital beds have excess lengths of stay and could be looked after in an alternative setting. See how UK health policy is shifting towards more care being provided out of the acute hospital setting.
Part 2
Evidence suggests that Out of Hospital healthcare when delivered well, can provide considerable benefits for both patients & integrated care providers.
Part 3
For Out of Hospital care models, the BHF’s pilot programme evaluating the treatment of heart failure patients in the community with intravenous diuretics delivers some fantastic results.
Part 4
Facilitating Out of Hospital care with the right line, right patient, right time in the right setting supports early discharge and hospital avoidance pathways, providing a wide range of benefits.
Learning From Past Successes
There are many examples of effective integrated OOH care pathways. These include Hospital at Home, Virtual Hospitals, Acute Care at Home, OPAT services and Hospitals without Wards. Treatments provided include, but are not limited to:

Working in Partnership:
By replicating previous successes and modifying existing pathways, the process of acute to OOH care can be effectively implemented for a wider patient demographic.
Vygon is continuing to support the seamless delivery of healthcare across care settings by developing a range of products, services, training programmes, and methods. Our aims are the same; shorter inpatient bed days, more effective patient flow through the hospital, and a quicker, safer discharge into the community setting.
The setting up of an Outpatient Parenteral Antibiotic Therapy (OPAT) service at London’s Homerton Hospital in 2014 has delivered a raft of benefits for both the Trust and patients.
Vygon was at the heart of an initiative with the Royal Devon & Exeter NHS Foundation Trust to deliver care at home.
Vygon’s Support
The pathway from the acute setting to OOH healthcare takes many cogs to make the wheel turn. At Vygon, we have worked with healthcare providers to deliver community-based IV services for 20 years, providing a partnership that supports this pathway.
OOH pathways facilitate the delivery of integrated care between acute and community services and ensures continuity of care. The promotion of hospital admission avoidance or early discharge programmes, allowing a patient to receive their care in an alternative setting, requires a multi-disciplinary approach. Key components in this process include having the right vascular access device for the right patient at the right time that allows safe and efficient delivery of therapy whilst promoting vessel health and preservation, as well as appropriate care and maintenance of the device.

At Vygon, we offer a range of vascular access products and services, including training and educational programmes, to support you in offering treatment and delivery of care in the most appropriate location for your patient's needs. Ultimately, it is about making the best use of resources to improve health and wellbeing outcomes.
To find out how Vygon can support you in delivering your OOH pathway, contact us below:
For more information please contact us
References
- Nuffield Trust: Shifting the Balance of Care – Great Expectations, Mar 20-17. Available on-line: https://www.nuffieldtrust.org.uk/research/shifting-the-balance-of-care-great-expectations
- Age UK (2017) Available on-line: https://www.ageuk.org.uk/latest-press/articles/2017/october/four-million-hospital-bed-days-lost-since-2011-due-to-problems-securing-social-care/
- NHS Long Term Plan June 2019. Available on-line: https://www.longtermplan.nhs.uk/
- The Kings Fund – Specialists in Out of hospital settings: findings from six case studies Oct 2014 Available online :https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/specialists-in-out-of-hospital-settings-kingsfund-oct14.pdf
- HFMA Briefing - The Value of Community Services: comparison with acute settings Mar 2019 Available online: https://www.hfma.org.uk/docs/default-source/publications/Briefings/the-value-of-community-services---comparison-with-acute-settingsc63f0ace1ab7692cb427ff0000b8cb05.pdf?sfvrsn=2
- Munton T, Martin A, Marrero I, Llewellyn A, Gibson K, Gomersall A (2011) Getting out of hospital? The evidence for shifting acute inpatient and day case services from hospitals into the community The Health Foundation.
- Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L, Ricauda NA, Tibaldi V, Wilson AD (2009a). Avoiding hospital admission through provision of hospital care at home: a systematic review and meta-analysis of individual patient data. Canadian Medical Association Journal 20:180 (2), 175-182.
- Shepperd S, Doll H, Broad J, Gladman J, Iliffe S, Langhorne P, Richards S, Martin F, Harris R (2009b) Early discharge hospital at home. Cochrane Database of Systematic Reviews. 21 (1): CD000356.