Oxygen Therapy: Too much is bad | Article Summary

Benefits and harms of supplemental oxygen administration in ICU for critically ill patients
Article featured in ICU management and practice. Bruno Pastene and Marc Leone, Department of and Intensive Care Unit, Hospital Nord Assistance Publique Hôpitaux de Marseille.
Article overview
Oxygen is administered routinely in ICU settings, but are we considering all the risks?
In this article Bruno Pastene and Marc Leone explore the existing literature on the benefits and harms of supplemental oxygen administration in ICU for critically ill patients. They highlight that across clinical studies and found that across clinical studies, there are inconsistencies in the definition of hyperoxia which has led to inconsistencies in findings. (Barbateskovic et al. 2019; Damiani et al. 2014).
Increasing evidence suggests that exposure to hyperoxia during critical illness is associated with impaired outcomes and that conservative oxygen therapy should be a future recommendation in most guidelines. (Barbateskovic et al. 2019; Chu et al. 2018).
“Whereas hypoxia may be viewed as a natural response to injury, hyperoxia is never found except in conditions generated by human interventions. In this sense, oxygen should be assessed as a drug with possible side effects in case of overdosage.”
(B. Pastene, M. Leone 2021)
Risks of Hyperoxia
Pastene and Leone also explore the reported risks of hyperoxia from several randomised trials studied the effects of prolonged hyperoxia by reporting mortality rates in patients treated with a liberal oxygen therapy compared to patients treated with conservative strategy. This was also compounded by studies on the effects of hyperoxia on different indications such as sepsis, post- cardiac arrest, brain injuries and chest trauma.
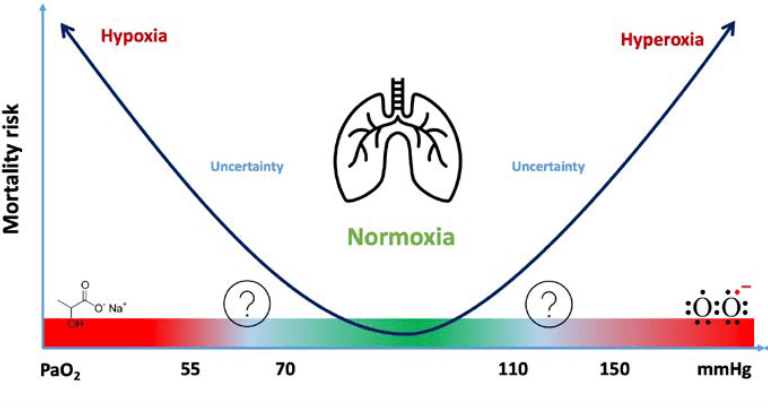
These trials concluded that although the risks associated with hypoxemia are great, there are also poor outcomes associated with the administration of high levels of oxygen including increased mortality risks.
Conclusion
In critically ill patients, the trend is to administer high levels of oxygen to counteract the risks of hypoxaemia. This can lead to poor patient outcomes, and it is important to ensure oxygen is not used unnecessarily or administered longer than required. Recommendations are to adopt a less is more strategy and develop personalised approaches to keep patients within the safe zone of the U-shaped curve of hypoxaemia and hyperoxia (Figure a).
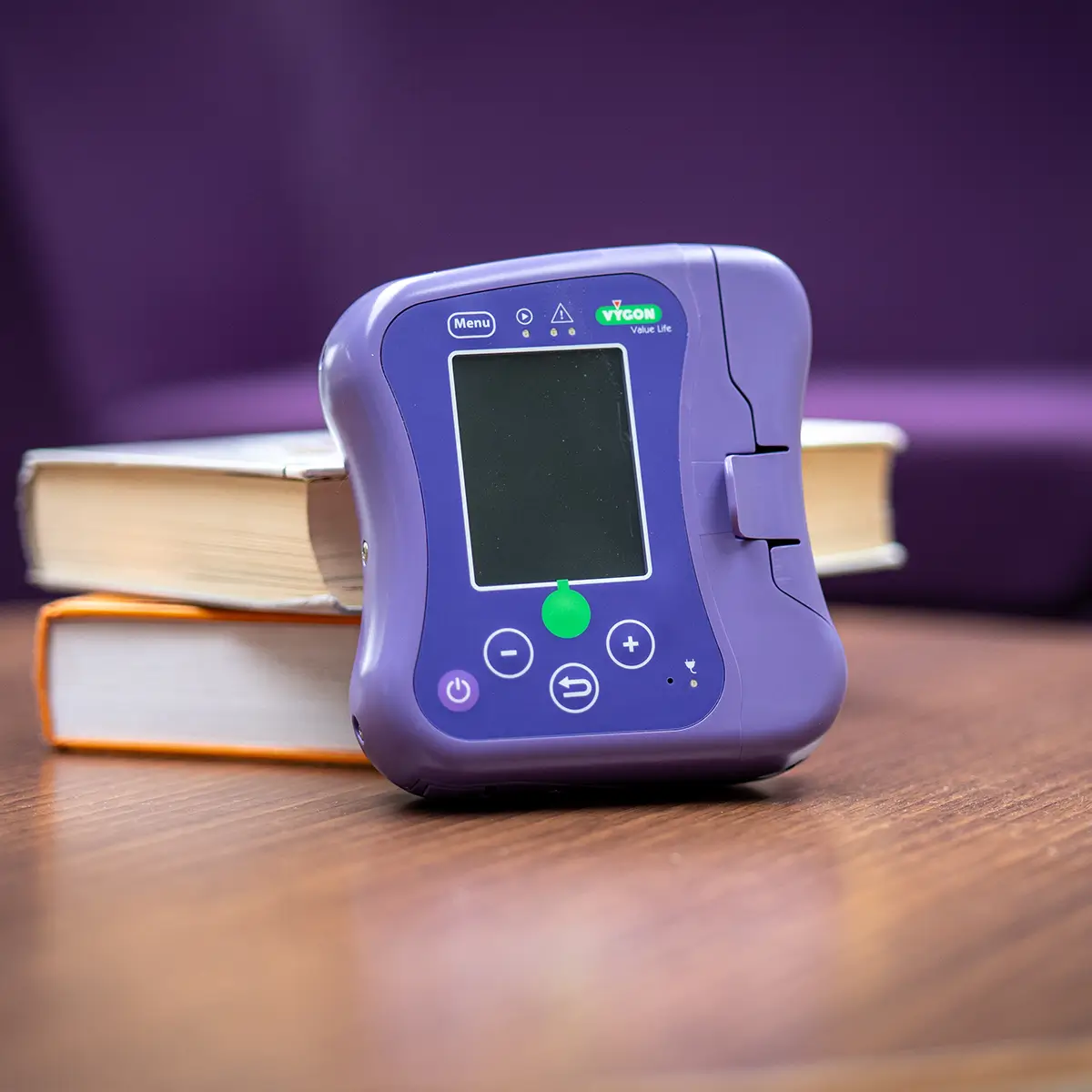
Reduce the Risks of Hyperoxia with Automated Oxygen Therapy with Free O2
The FreeO2 Automated Oxygen Therapy Device is not dependant on manual intervention by a healthcare professional, instead it provides oxygen therapy on demand, based on continuous, non-invasive monitoring of oxygen saturation.
FreeO2 will maintain the patient’s oxygen within predetermined levels, and automatically adjusts flow rates and delivery to maintain target oxygenation (SpO2). By using automated oxygen therapy the risk of complications relating to hypoxia and hyperoxia are reduced significantly.
Find out more
Follow the button below to request the full paper, or to find out more about how to reduce the risks of hyperoxia through automated oxygen therapy please email marketing@vygon.co.uk .
Benefits of FreeO2
Patient benefits
Reduced complications
Healthcare workers
Safer, more effective and more efficient
Trust benefits
Faster recovery and reduced length of stay
Oxygen Delivery & Management for COPD Patients
In a study of chronic obstructive pulmonary disorder (COPD) patients, the use of FreeO2 resulted in more effective oxygenation and limited complications as a result of hypoxia and hyperoxia. This resulted in the patients spending 30% less time in hospital.
To talk to one of our team about any case studies, and the clinical benefits on patient outcomes, email marketing@vygon.co.uk