Oxygen Therapy in Critical care

When do you need oxygen therapy?
Acute respiratory distress syndrome (ARDS) or respiratory failure are common conditions and can be costly and even deadly if not treated effectively.
Acute Respiratory Failure is defined as “The loss of the ability to ventilate adequately or to provide sufficient oxygen to the blood and systemic organs. The pulmonary system is no longer able to meet the metabolic demands of the body with respect to oxygenation of the blood and/or CO2 elimination.”[1]
ARDS is commonly split into two classifications, which are classified according to blood gas values (PaO2)
Type 1 (Hypoxemic ) (PaO2) <60 mm Hg. Usually seen in patients with an acute lung injury or infection which causes the lungs to become severely inflamed and prevents adequate oxygenation of the blood.
Causes of type 1 respiratory failure include: pulmonary oedema, pneumonia, COPD, asthma, acute respiratory distress syndrome, chronic pulmonary fibrosis, pneumothorax, pulmonary embolism, pulmonary hypertension.
Type 2 (Hypercapnic) - PaCO2 > 45 mmHg. At its root, hypercapnia is caused by either increased CO2 production metabolically or Respiratory failure. Respiratory failure in this pathology is a failure to eliminate CO2 from the pulmonary system, which is synonymous with hypoventilation secondary to decreased respiratory rate or decreased tidal volume[1].
A common cause of type 2 respiratory failure is COPD but other causes include chest-wall deformities, respiratory muscle weakness and Central nervous system depression (CNS depression.)
Respiratory function can be impaired post-operation and a common side effect of general anaesthesia and surgery is hypoxia[2]. Post- operative respiratory failure is the most common Postoperative pulmonary complication (PPC)[3] and can be both costly to treat and can increase patient mortality.
Critically ill patients need close monitoring to ensure they remain within the target range of oxygen saturation and prompt intervention is required if the levels fall outside of this. These targets are patient-specific, especially those at risk of hypercapnic respiratory failure[4] such as COPD patients. However, in clinical practice, the manual and sporadic adjustment of oxygen flow rates make it difficult to achieve precise control on the oxygen levels as well as being time consuming, this often results in higher than necessary levels of oxygen being administered, thus prolonging the duration of oxygen therapy and therefore the patient’s length of stay.
How do you administer oxygen therapy?
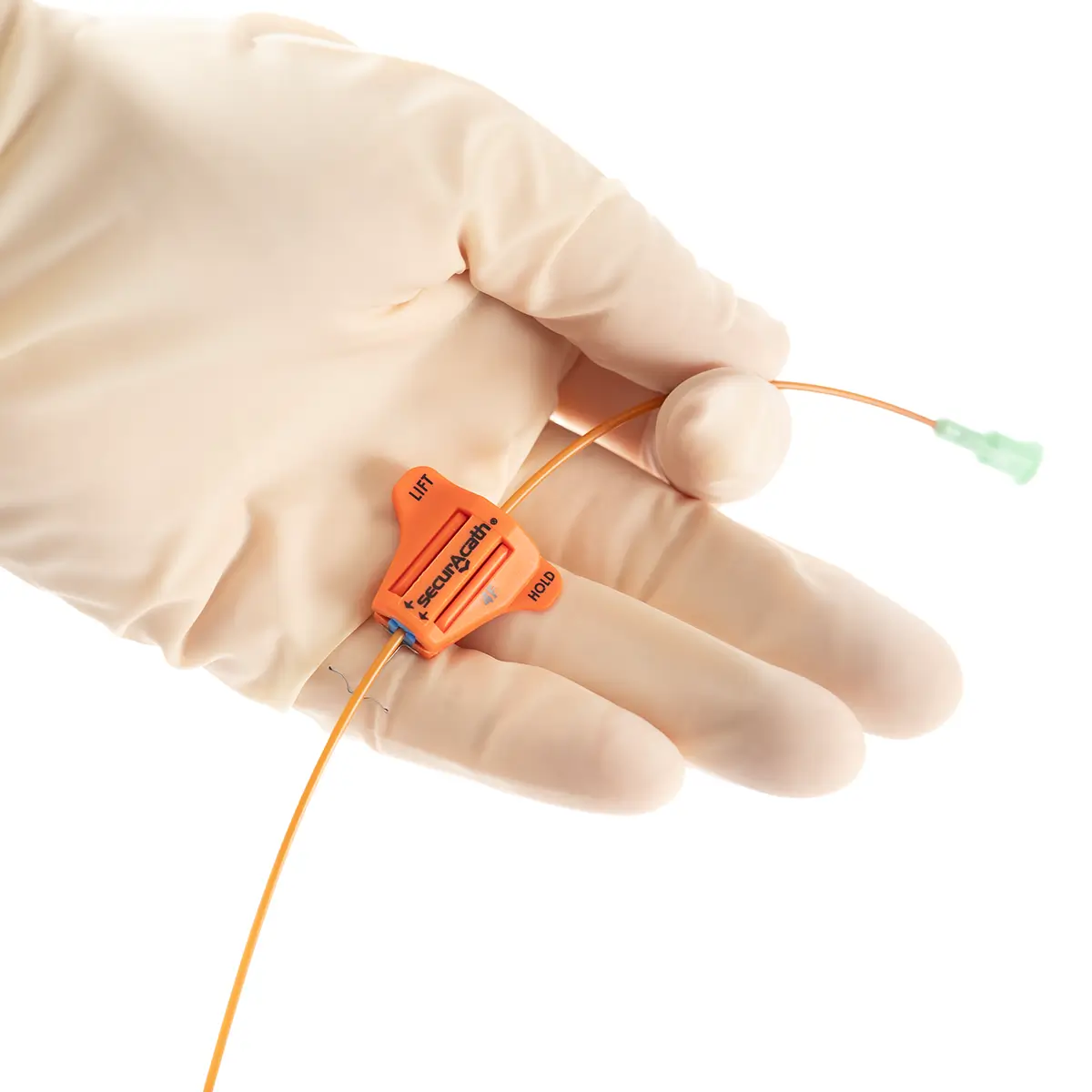
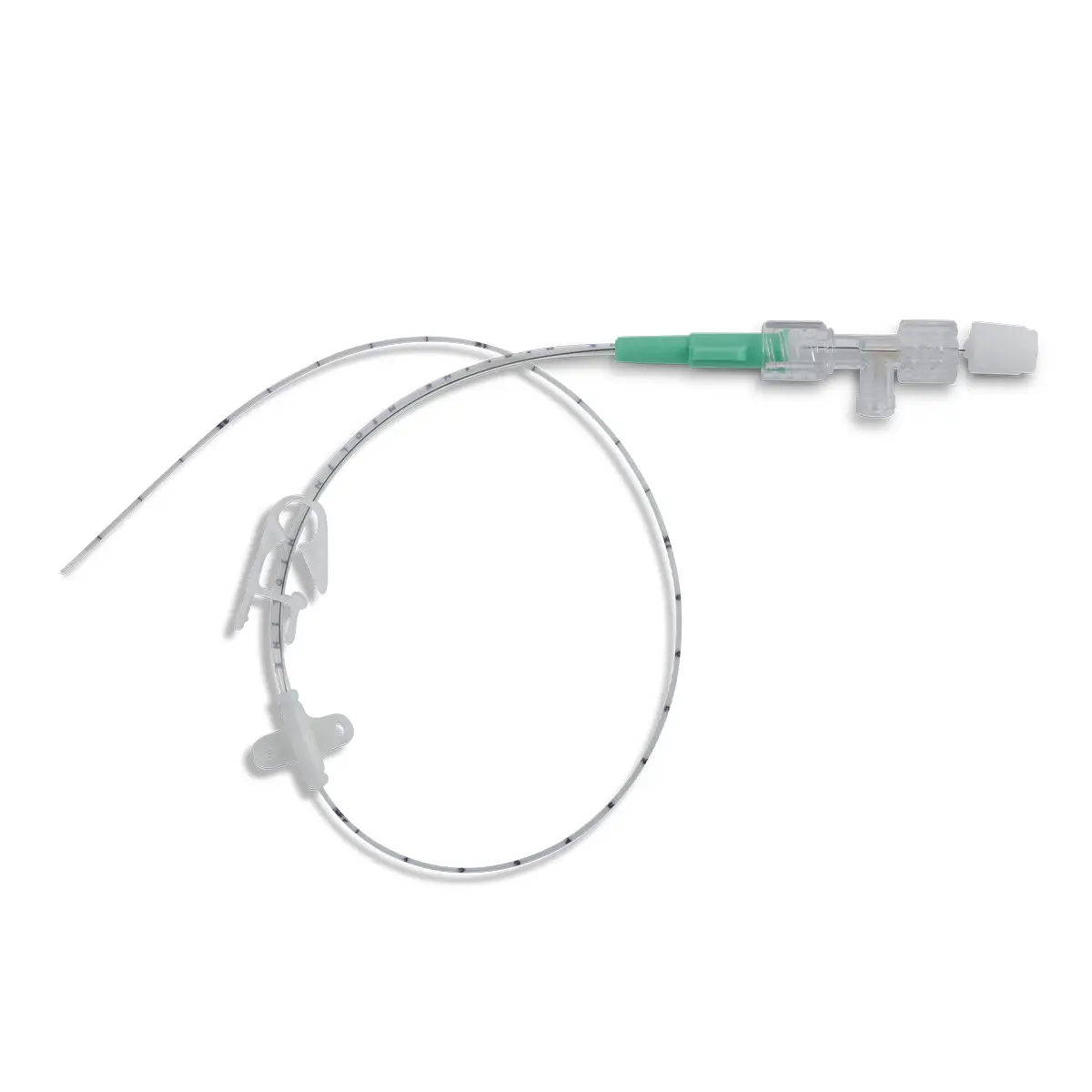
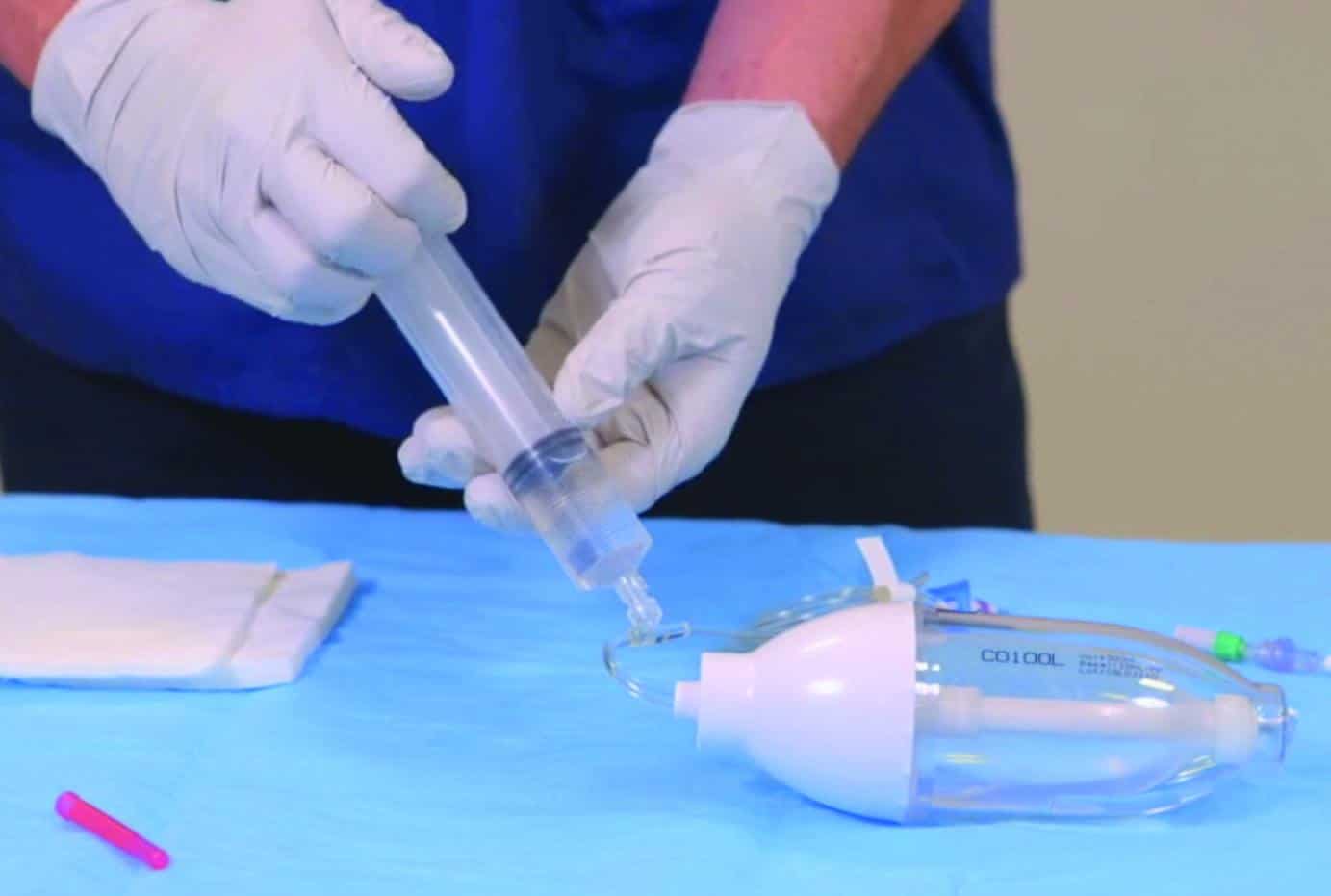
Oxygen therapy is first-line treatment for hypoxaemic acute respiratory failure (ARF). Conventional oxygen therapy is delivered via nasal cannulae (NC) or face masks (FM). It is a non-invasive method and oxygen saturation levels are adjusted to maintain at 90% or more as measured by pulse oximetry (SpO2), until the patient recovers.
High-flow nasal oxygen therapy (HFNO) represents an alternative to conventional oxygen therapy and provides humidified, titrated oxygen therapy matching or even exceeding the patients' inspiratory demand[5]
When administering high-flow nasal oxygen (HFNO) to patients in acute respiratory distress, staff must consider if the patient will need transferring from an emergency department or short-stay unit, and an appropriate device must be used to deliver the patients oxygen. This is due to the majority of HFNO delivery devices requiring mains power and even brief interruptions could lead to respiratory and cardiac arrest.[6]
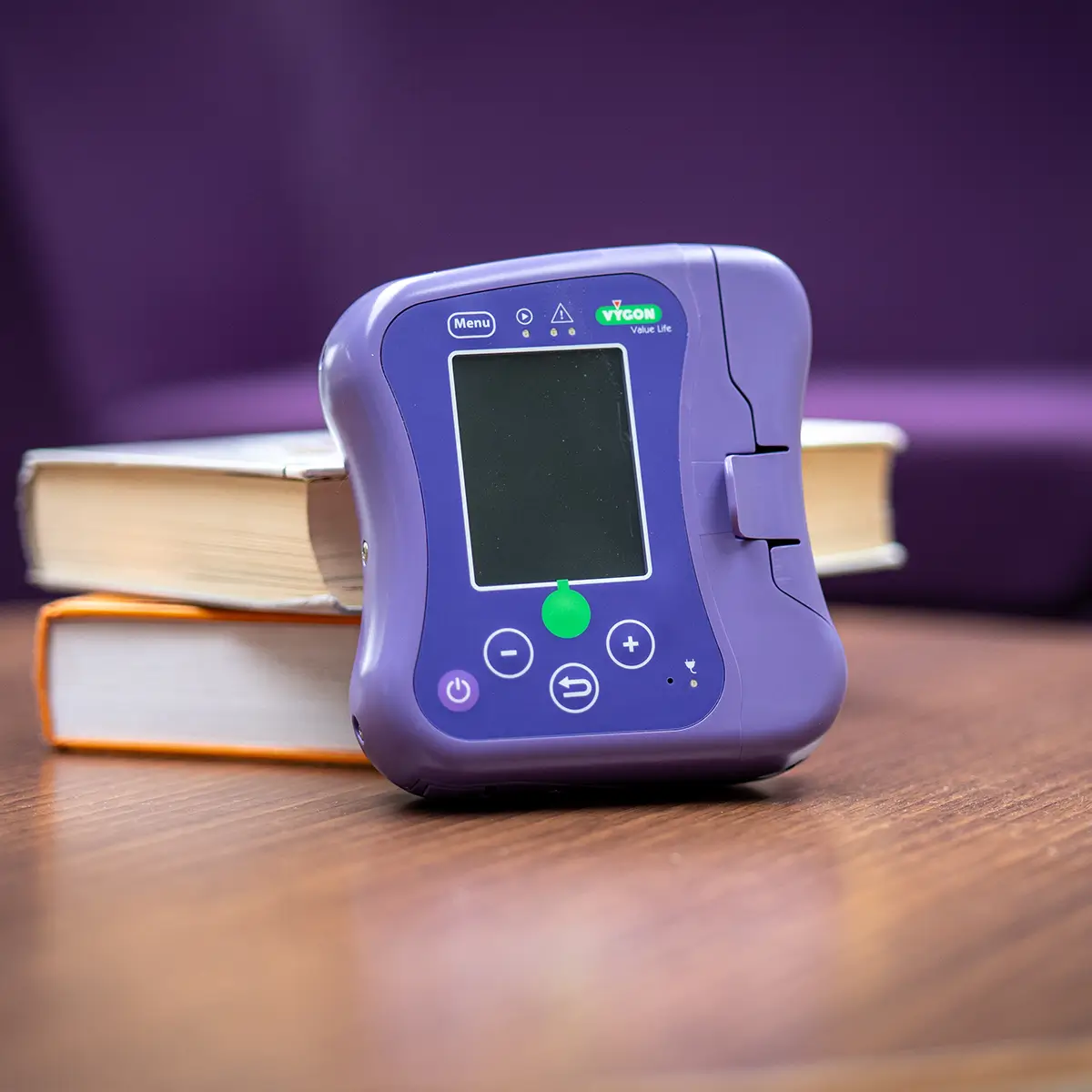
Benefits of FreeO2
FreeO2 is a lightweight portable device that can be used with a nasal cannula or face mask and can deliver oxygen at a flow rate of 0-20L/min.
By continuously and automatically adjusting each patient’s oxygen flow, regardless of age group (paediatric or adult), the device accounts for individual needs and dynamics to help them remain within the target SpO2 set by the clinician. The patient is then treated according to their specific needs, and the risks of complications from hypoxemia and hyperoxia are reduced.
By limiting complications related to hypoxemia and hyperoxia, FreeO2 enables certain patients to be weaned more quickly, avoid transference to intensive care, and reduce length of stay. By treating patients more effectively there is a reduction of healthcare staff’s workload and greater adherence to clinical protocol.
FreeO2 in Practice
FreeO2 is proven to limit complications such as hypoxia and hyperoxia and therefore reduced time COPD patients spent in hospital by 30%
Over 500 COPD patients have been involved in clinical trials and studies using the FreeO2 monitor.
Outcomes showed optimum oxygen saturation was improved by 56%, equating to a 21% cost saving.
To find out more about how Vygon UK can help your Trust with respiratory services, get in touch today.